Simply Stated: Research Updates in Emery-Dreifuss Muscular Dystrophy (EDMD)
By Sujatha Gurunathan | Friday, April 28, 2023
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
Emery-Dreifuss muscular dystrophy (EDMD) is a rare genetic disorder that affects muscle and joint function, and is often associated with cardiac (heart) complications. The exact prevalence of EDMD is unknown, but the most common form of the disease is estimated to affect about 1 in 100,000 people worldwide.
Symptoms of EDMD
Many people with EDMD begin experiencing symptoms by the age of 10 years old, though symptoms can appear as late as the mid-20s. Progression of EDMD is typically slow, but the onset of symptoms, severity, and progression of disease can vary greatly between different people, even within the same family.
In general, EDMD causes gradual weakening and atrophy (loss) of the muscles in the shoulders, upper arms, and lower legs. Contractures (stiff joints) are also common early in the course of disease, making arm, neck, heel, and spine movements difficult. As a result, people with EDMD may exhibit “toe-walking” because of stiffness in the Achilles’ tendons in their heels, as well as difficulty bending their elbows. Most people with EDMD retain the ability to walk for many years, though certain forms of EDMD (e.g., autosomal dominant EDMD) are more likely to affect walking ability. Symptoms of EDMD typically progress slowly during the first three decades of life, and then advance more rapidly later in life.
Cardiac problems, including conduction abnormalities (problems with the heart’s electrical system) and dilated cardiomyopathy (weakening and enlargement of the heart), are common in people with EDMD in the second or third decade of life. These cardiac problems can be life-threatening, but are often manageable with proper treatment.
Cause of EDMD
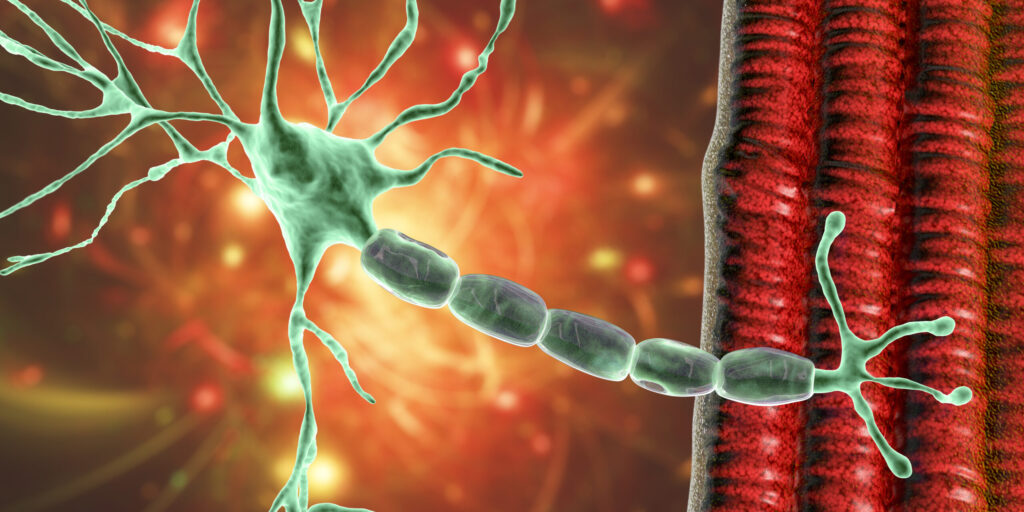
Researchers have identified several genes that, when defective, lead to forms of EDMD. Most of these identified genes encode proteins in the membrane surrounding the cell’s nucleus (structure that holds the cell’s genetic information). These include the EMD gene which is found on the X chromosome and encodes the nuclear membrane protein emerin. Defects in the EMD gene cause the X-linked form of EDMD, which is inherited from the mother and primarily affects males. Another form of EDMD is caused by the LMNA gene, which encodes the nuclear membrane proteins lamins A and C. Defects in the LMNA gene are responsible for a form of EDMD that can be inherited from either parent and is usually inherited in a dominant way, meaning that only one copy of the defective gene is enough to cause the disease (known as autosomal dominant EDMD). In addition to EMD and LMNA, a handful of other genes have also been implicated in EDMD. In many cases, however, the genetic defect that causes EDMD is not known. Of note, some women who are genetic carriers for X-linked EDMD may be at risk for cardiac problems, though they rarely experience the muscular weakness associated with EDMD.
Diagnosis of EDMD
EDMD can be difficult to diagnose; the symptoms can be variable and may be mistaken for other neuromuscular conditions, including other inherited muscular dystrophies or myopathies, as well as a condition known as rigid spine syndrome (RSS). An EDMD diagnosis is typically based on a combination of clinical symptoms and genetic testing. Some clinical features that may suggest a diagnosis of EDMD include:
- Early contractures of the muscles of the elbow, ankle, and spine
- Childhood onset of weakness in the shoulders, upper arms, and lower legs
- Cardiac problems such as conduction defects, arrhythmias (irregular heartbeat), and cardiomyopathy
A specialized genetic test performed in a diagnostic laboratory is required to detect the genetic defects that cause EDMD and may be a prerequisite for enrollment in clinical trials. Genetic counseling and testing are important for individuals with a family history of EDMD or for those who are at risk of passing the condition on to their children.
Current management of EDMD
There is currently no known cure or disease-modifying therapy for EDMD. However, several therapies and strategies are available that can help manage the symptoms and improve the overall health of people with EDMD. These may include:
- Physical therapy focused on stretching exercises to prevent the early development of contractures
- Orthopedic procedures to release contractures
- Spinal fusion for severe scoliosis
- Walking aids (e.g., canes walkers, orthoses, wheelchairs) to facilitate mobility
- Respiratory aids in the late stages of the disease (rarely needed)
To manage cardiac problems, people diagnosed with EDMD should be monitored regularly for development of conduction defects or signs of cardiomyopathy. Interventions such as a placement of a pacemaker or implantable defibrillator may be required to treat arrhythmias, cardiomyopathy, and conduction defects. Medications may also be prescribed to treat cardiomyopathy.
Given the variability of disease progression and symptoms experienced by different people with EDMD, treatment plans are typically individualized to meet the needs of the affected person and may include recommendations from a variety of specialists.
Evolving research and treatment landscape
It is not yet understood how defects in nuclear membrane proteins cause EDMD or why the symptoms of EDMD are restricted to muscle cells. These questions form the basis of ongoing pre-clinical research.
While the standard of care is still symptom management, understanding of EDMD progression and the genetic elements that cause EDMD will likely guide the development of new treatment strategies.
Several observational studies are underway to better understand these aspects of the disease.
To learn more about clinical study opportunities in EDMD, visit clinicaltrials.gov and search for “Emery-Dreifuss muscular dystrophy” in the condition or disease field.
MDA’s work to further cutting-edge EDMD research
MDA is committed to furthering research in and therapeutic development for EDMD, and has funded about $1 million in EDMD research grants since 2014. Funded projects include:
Assessing the role of fibro-adipogenic progenitors in EDMD (2022-2025)
Dr. Chiara Mozzetta, CNR-Institute of Molecular Biology and Pathology
This project focuses on fibro-adipogenic progenitors (FAPs), a population of muscle-resident cells that support the formation of new muscle, but also give rise to fibrotic (involved in scarring) and fat cells that accumulate in degenerating muscles. The goal is to study whether FAPs play a role in EDMD caused by lamin A/C defects, and to determine if they might represent a new therapeutic target to block the muscle cell loss and scarring that occur in EDMD muscles.
Advanced heart failure therapy outcomes in neuromuscular cardiomyopathy (2022-2025)
Dr. Forum Kamdar, Regents of the University of Minnesota – Twin Cities
This project combines data from large muscular dystrophy and advanced heart failure centers to look at the outcome and survival of people with muscular dystrophies who undergo heart transplant or heart pump treatment. Little is known about the utility of these procedures in people with multi-system diseases such as muscular dystrophy, so this work has the potential to address a gap in the current heart care of people with NMDs.
DNA-PK hyperactivation in the progression of Emery-Dreifuss muscular dystrophy (2019-2022)
Tyler Kirby, VU University Medical Center Amsterdam
This project studied how the loss of the lamin A/C proteins contributes to disease in EDMD. The researchers tested the hypothesis that loss of lamin A/C makes the cell nucleus vulnerable to the forces generated within muscle, resulting in physical damage to the nucleus and the DNA inside. They also tested whether pharmacological inhibition of a specific DNA repair protein, DNA-PK, can slow disease progression in an animal model. The goal was to further the understanding of EDMD with the hope of developing more effective treatments.
Suppression of lamin-induced muscle defects (2017-2020)
Lori Wallrath, The University of Iowa
This project aimed to identify potential treatments for EDMD. The researchers used the fruit fly genetic model, as well as EDMD patient-derived cells, to identify and test potential drug candidates. Preliminary data showed that muscle function can be restored in a fruit fly model of EDMD, demonstrating feasibility of this approach.
Emerin-LAP1 interaction and X-linked Emery-Dreifuss muscular dystrophy (2014-2017)
Howard J. Worman
In this project, researchers worked to create a better mouse model of EDMD that more closely resembles human disease. By deleting both emerin and LAP1, and protein that interacts with emerin in the muscle, in engineered mice, they were able to produce animals that develop muscular dystrophy and heart disease, mimicking the symptoms of X-linked EDMD. These mice will be used to study abnormalities in muscle and test potential new treatments for X-linked EDMD.
Together, these studies are helping researchers to better understand this rare disease and to identify new targets for therapeutic intervention. They will lay the groundwork for future clinical trials, thereby improving prospects for better disease management for people living with EDMD.
MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about Emery-Dreifuss muscular dystrophy, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
Next Steps and Useful Resources
- MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about Emery-Dreifuss muscular dystrophy (EDMD), open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org
- For more information about the signs and symptoms of Emery-Dreifuss muscular dystrophy (EDMD), as well an explanation of the causes of disease, an in-depth overview can be found here.
- To learn more about clinical study opportunities in EDMD, visit clinicaltrials.gov
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Clinical Trials, Drug Development, Gene Therapy, Simply Stated
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




