Simply Stated: Updates in Ryanodine Receptor 1-Related Disorders (RYR-1-RD)
By Sujatha Gurunathan | Thursday, May 29, 2025
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
RYR-1-Related Disorders (RYR-1-RD) are a group of rare, inherited muscle disorders caused by variants in the RYR1 gene. This gene encodes the ryanodine receptor type-1 (RyR1) protein, which is important for muscle function and the ability of muscles to contract. People with RYR-1-RD experience muscle weakness, and may exhibit a variety of other symptoms, including a potentially life-threatening reaction to anesthesia called malignant hyperthermia. RYR-1-RD is considered the most common form of congenital myopathy, and it affects approximately 1 in 90,000 people in the United States.
Cause of RYR-1-Related Disorders (RYR-1-RD)
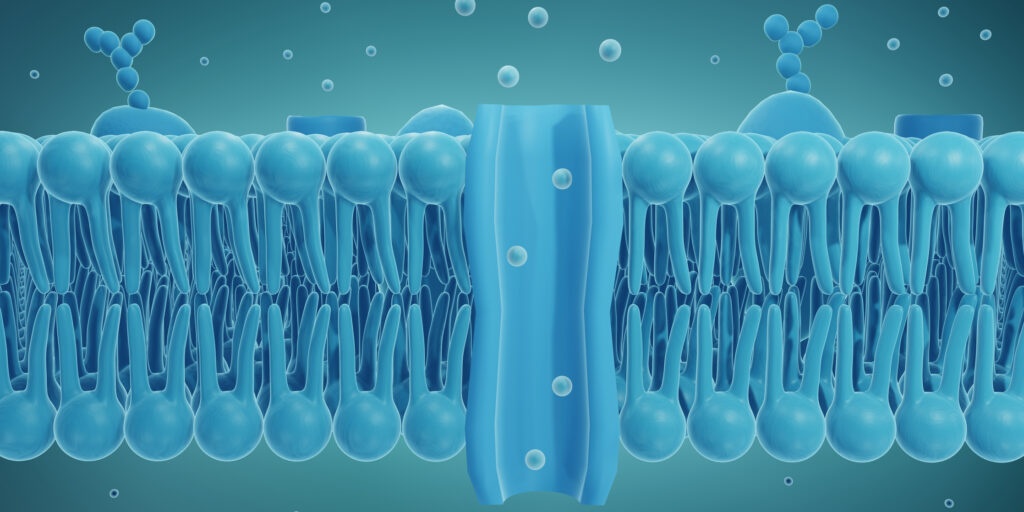
RyR1 proteins are typically located in skeletal muscle cells and function as channels that control the release of calcium, which is needed for muscles to contract. When the nervous system sends a signal, the RyR1 channels open and allow calcium to be released from a special compartment in the muscle (the sarcoplasmic reticulum) into the other parts of the muscle cell. This release of calcium triggers skeletal muscles to contract and produce force or movement. In RYR-1-RD, a variety of changes to the RYR1 can occur, including 1) too much calcium being released, 2) An insufficient amount of calcium being release, 3) A chronic calcium “leak” resulting in a gradual loss of calcium from internal stores in the cell, and 4) A reduced number of RyR1 channels. The specific change to the RyR1 channel is determined by the specific variant in a patient’s RYR1 gene. These changes to the RyR1 channel result in varying types and severities of muscle weakness and dysfunction that can be seen in RYR-1-RD.
To date, hundreds of RYR1 gene variants have been identified, however, it is not clear how many of these variants actually cause disease. The different RYR1 gene variants can lead to alterations in the number, structure and/or function of RyR1 channels. Furthermore, RYR-1-RD can be inherited in a dominant (caused by one copy of the RYR1 gene variant) or recessive (caused by two copies of the RYR1 gene variant) manner or can develop due to spontaneous (de novo) RYR1 variants. The wide range of genetic causes and inheritance patterns in RYR-1-RD helps explain why the age of onset, symptoms, and disease severity can differ so much from person to person.
Types and symptoms of RYR-1-Related Disorders (RYR-1-RD)
RYR-1-RD include many different muscle conditions that are caused by variants in the RYR1 gene. These conditions can vary greatly in symptoms, even within the same family. They are often more severe when inherited recessively, though this is not always the case. Common muscle-related symptoms include weakness in the eye, face, and proximal (close to the body center) muscles, muscle pain, heat and exercise intolerance, and cramping. Breathing problems can occur due to weakness in respiratory muscles, and can sometimes necessitate breathing support. People with RYR1 variants are also at risk for malignant hyperthermia and some may experience exertional rhabdomyolysis, a condition in which muscles break down after exercise or illness.
Historically, many RYR-1-RD were classified by histopathology, or how affected muscle tissues looked under a microscope. Major subtypes that were classified in this way include:
Central Core Disease (CCD)
● The most common RYR-1-RD
● Usually causes mild to moderate muscle weakness, especially in the hips and legs
● Characterized by “cores” seen in muscle biopsies (areas lacking mitochondrial enzymes)
● Can be inherited in dominant or recessive patterns
Multi-minicore Disease (MmD)
● Often caused by variants in either the RYR1 or SEPN1 genes
● Is typically more severe than CCD
● Symptoms include weakness in facial, neck, and respiratory muscles, abnormal curvature of the spine
● Multiple small lesions or “minicores” seen in muscle biopsy
● Often inherited in a recessive pattern
Centronuclear Myopathy (CNM)
● Characterized by centrally placed, rather than peripheral, nuclei (structures that contain DNA) in muscle fibers
● Commonly caused by variants in the RYR1, MTM1, or DNM2 genes
● Symptoms include muscle weakness, droopy eyelids (ptosis), eye movement problems
Congenital Fiber-Type Disproportion (CFTD)
● Characterized by type 1 (slow-twitch) muscle fibers being smaller than type 2 (fast-twitch) muscle fibers
● Typically causes mild to moderate weakness, especially in the muscles of the face, shoulders, hips, upper arms, and thighs
● Commonly caused by variants in the RYR1, ACTA1, TPM3, or SEPN1 genes
Over the years, additional disorders linked to RYR1 variants have been described based on their clinical symptoms. Some of these disorders include the following:
Malignant Hyperthermia Susceptibility (MHS)
● A potentially life-threatening reaction to certain anesthesia drugs (e.g., halothane, succinylcholine)
● Characterized by a sudden rise in body temperature and metabolism, muscle rigidity, and increased heart rate
● Is not always associated with muscle weakness
● Can be associated with increased muscle strength and athleticism
Exertional Rhabdomyolysis
● Sometimes associated with RYR1 variants, but can result from other causes
● Muscle breakdown triggered by intense exercise, heat, or illness
● Can occur in people with or without baseline muscle weakness
● Symptoms include muscle pain, dark urine, risk of kidney damage
King-Denborough Syndrome
● Rare and severe condition
● Features include susceptibility to malignant hyperthermia, skeletal abnormalities, and muscle weakness
● Often diagnosed in early childhood
Adult-Onset RYR1 Myopathy (RYR1-RM)
● Muscle weakness that starts in adulthood
● Often milder and progresses slowly
● May be confused with other types of muscular dystrophy
The various RYR-1-RD can present with overlapping symptoms, making diagnosis and management challenging. For more information about the types and characteristic symptoms of RYR-1-RD, as well as an overview of diagnostic and management concerns, an in-depth overview can be found here.
Diagnosis and current management of RYR-1-Related Disorders (RYR-1-RD)
A RYR-1-RD may be suspected based on clinical signs and symptoms as well as family history. In this case, further testing will likely be recommended. This may include muscle biopsy, muscle MRI, and genetic testing. Gene sequencing to identify specific changes in the RYR1 gene and gene panels to identify other contributing genes, such as SEPN1, can help to reach a definitive diagnosis.
Current strategies to manage RYR-1-RD are designed to alleviate signs and symptoms, but do not fix the underlying cause of disease. Multidisciplinary care focused on monitoring symptoms, providing supportive care, and preventing complications can help improve the quality of life and activities of daily living for affected people. The care team for a person with a RYR-1-RD may include a neurologist, pulmonologist, orthopedist, physical and occupational therapists, speech-language pathologist, and genetic counselor, among other specialists.
Importantly, steps can be taken to prevent the triggering of Malignant Hyperthermia (MH) in a person with RYR1 variants. An affected person should wear a medical alert bracelet, notify their healthcare providers of the genetic condition, and avoid exposure to certain anesthesia medications. If an RYR-1-RD patient requires anesthesia, the care team should be advised to take “MH precautions.” If an episode of MH is triggered, then the muscle relaxant dantrolene may be given to block excessive calcium release and blunt the dangerous symptoms of MH.
Evolving research and treatment landscape
There are still many unmet needs for people with RYR-1-RD. Although effective therapies have not yet been developed, a couple of clinical trials have tested new therapies to treat these conditions. These include:
ARM 210 (Surlorian formerly RyCals) (RyCarma Therapeutics formerly ARMGO Pharma, Inc.) – A small molecule designed to bind to and stabilize leaky RyR channels and restore normal calcium signaling in cells. This therapy showed preliminary evidence of safety and effectiveness in a phase 1 trial completed in 2023.
N-acetylcysteine (NAC) (National Institute of Nursing Research (NINR)) – Antioxidant therapy designed to reduce damaging oxidative stress, which can be caused by increased calcium levels in the cell. This therapy showed promise in preclinical models and a phase 1/2 trial completed in 2018.
It is important to note that these therapies remain in the early stages of development and are not yet widely available. However, they represent promising advancements in the field, with the potential to improve treatment options for RYR-1-RD.
In addition to emerging therapies, patient registries and observational studies are being established to help collect and analyze data from people with RYR-1-RD in order to improve understanding of these diseases. One such opportunity is:
A Natural History Study of RYR1-Related Disorders (National Institutes of Health Clinical Center (CC)) – In this study, researchers are seeking people aged 7 years and older with an RYR-1-RD to participate in non-invasive testing, activity tracking, and quality of life questionnaires. This observational study is currently recruiting participants. People interested in participating can contact the NIH Office of Patient Recruitment by telephone (800) 411-1222 or email ccopr@nih.gov and reference Research Study #001737-CC.
To learn more about clinical trial opportunities in RYR-1-RD, visit clinicaltrials.gov and search for the disease name in the condition or disease field.
MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about RYR-1-related disorders, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
Next Steps and Useful Resources
- Thank you to the RYR-1 Foundation for providing resources and expertise to this article. They will host the RYR-1 Foundation International Family Conference 2025 on July 24 through July 27, 2025. The conference will be held at the Hyatt Regency Pittsburgh International Airport hotel. Register here.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




