Simply Stated: Updates in Endocrine Myopathies
By Sujatha Gurunathan | Tuesday, May 21, 2024
5 Second Summary
Simply Stated is a Quest series designed to simplify your neuromuscular disease journey with easy-to-understand facts about tests, treatments, scientific terms, and the latest research.
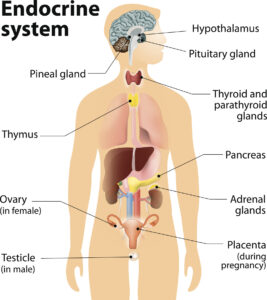
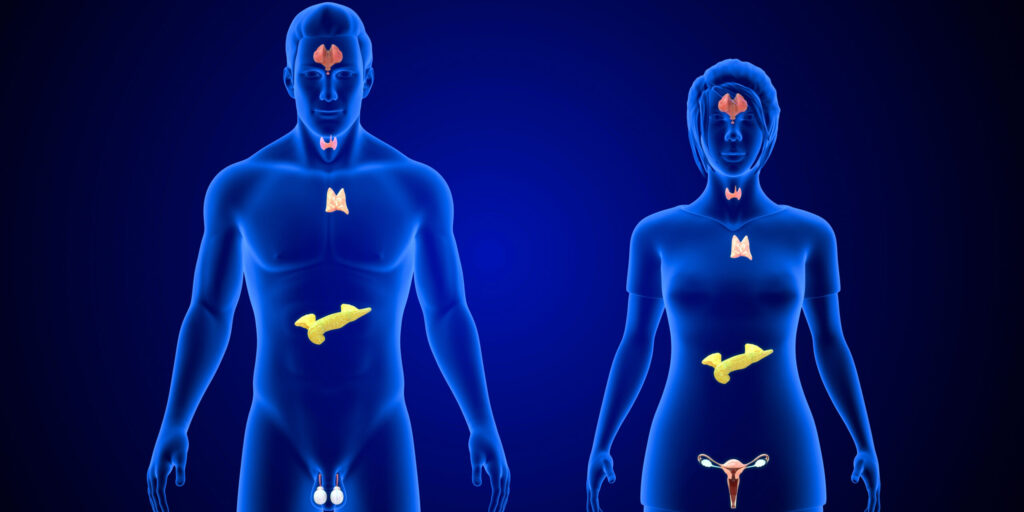
Endocrine myopathies are muscle disorders caused by abnormal activity of the endocrine (hormone-producing) glands, which include the thyroid, adrenal, parathyroid, pituitary, and gonadal glands. Too much or too little hormone production by these glands can cause weakness and atrophy (thinning) of the skeletal muscles that control voluntary movements. People with endocrine myopathies often experience symptoms such as generalized weakness and fatigue, which are also common in other neuromuscular conditions. In some cases, endocrine myopathies occur in response to other conditions or treatments/procedures that affect the function of the endocrine glands. As a result, the incidence of endocrine myopathy is often underreported or underdiagnosed, and the prevalence has been hard to estimate.
General overview of endocrine myopathies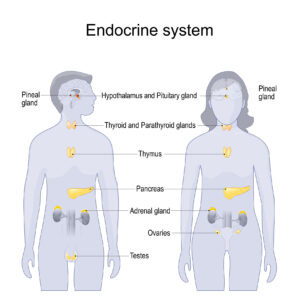
Myopathy (skeletal muscle disease) is a common side effect of endocrine disorders. People with endocrine myopathies often experience weakness and atrophy of the muscles around the shoulders and hips, as well as muscles stiffness, cramps, and slowed reflexes. In severe cases, they may also experience muscle breakdown. These conditions are usually not progressive, meaning they do not grow worse over time. Some children with myopathies may even gain strength as they get older.
The endocrine myopathies are not typically inherited. They are caused by an excess or a deficiency of hormones made by the endocrine glands. This can occur due to a genetic predisposition to another condition, such as an autoimmune disease, that causes damage to the endocrine glands. Alternatively, it can develop in response to a treatment or procedure, such as steroid administration or surgical removal of endocrine tissue, that impacts endocrine function. In some cases, dietary deficiencies can impact endocrine function.
The endocrine hormones regulate a number of critical processes in the body including metabolism (the process of changing food into energy) and protein synthesis and breakdown, among others. These processes are important for muscle function and integrity, which is why changes in endocrine function can sometimes lead to myopathy.
In general, the endocrine myopathies are highly treatable, using medication or surgery to restore normal hormone levels.
Types of endocrine myopathies
Thyroid myopathies
The thyroid gland is found in the neck of humans. It secretes two main hormones (triiodothyronine (T3) and thyroxine (T4)) that regulate metabolism, and thereby growth and development. Two different types of endocrine myopathies are caused by problems with the thyroid gland: hyperthyroid myopathy and hypothyroid myopathy.
Hyperthyroid myopathy
Symptoms: This type of endocrine myopathy usually occurs in adults and is caused by overproduction of thyroid hormones from the thyroid gland. The percentage of people with a hyperthyroid condition who go on to experience myopathy varies, with reports ranging from 50-80% of people. People with hyperthyroid myopathy often report muscle weakness and atrophy of the proximal muscles close to the body center (e.g., shoulders and hips), as well as muscle fatigue, which is sometimes described as exercise intolerance. Muscle weakness in the distal muscles far from the body center, and weakness in the face, throat, and respiratory (breathing) muscles can also occur.
In rare cases, an affected person may experience complications. These can include:
· Rhabdomyolysis – Severe muscle breakdown, which can be life-threatening
· Graves disease – An autoimmune disorder, which can lead to damage to eye and eyelid muscles and subsequent vision loss
· Thyrotoxic periodic paralysis – Acute attacks of muscle weakness associated with low serum potassium levels
Cause: Overactivity of the thyroid gland can occur for various reasons. One common cause is an underlying autoimmune condition that damages the thyroid gland.
Management: Hyperthyroid myopathy can usually be alleviated by reducing thyroid hormone levels through medication or by surgical removal of some or all of the thyroid gland.
Hypothyroid myopathy
Symptoms: This type of endocrine myopathy can occur in children or adults and is caused by underproduction of thyroid hormones from the thyroid gland. Depending on the study, 30-80% of people with a hypothyroid condition have reported experiencing myopathy. Common symptoms include proximal muscle weakness, muscle stiffness and cramping, and slow reflexes. In some cases, a phenomenon known as myoedema, in which a temporary lump forms in response to pressure on the muscle, can occur. Though rare, myoedema is a classical sign of hypothyroid myopathy. Rhabdomyolysis can also occur as a rare complication of hypothyroid myopathy.
Cause: A thyroid hormone deficiency can result from a lack of dietary iodine, which is essential to make the thyroid hormone. It can also occur in response to an autoimmune condition that damages the thyroid gland or, less commonly, following a treatment that affects the thyroid gland.
Management: Hypothyroid myopathy can usually be alleviated by restoring normal thyroid hormone levels through medication.
Parathyroid myopathies
The four small parathyroid glands are located behind the thyroid. These glands produce parathyroid hormone (PTH), which regulates calcium levels in the blood, impacting skeletal mineralization, or the process that strengthens and gives structure to our bones. Two different types of endocrine myopathies are caused by problems with the parathyroid gland: hyperparathyroid myopathy and hypoparathyroid myopathy.
Hyperparathyroid myopathy
Symptoms: This type of endocrine myopathy is caused by overproduction of PTH from the parathyroid gland. About one-fourth of people with overactive parathyroid function exhibit muscle problems. The most common symptoms are proximal muscle weakness, atrophy, and overactive reflexes (hyperreflexia), which can present as twitching or spasticity.
Cause: Overactivity of the parathyroid can result from abnormal growth (hyperplasia or adenoma) of the parathyroid glands. Alternatively, it can occur in response to kidney dysfunction that leads to buildup of waste products and imbalance of minerals and vitamins (e.g., phosphate, calcium, vitamin D) in the blood. These changes can also cause abnormal and even cancerous growth of the parathyroid, leading to overactivity.
Management: In some cases, myopathy that sometimes results from overactive parathyroid function can be alleviated by surgical removal of the parathyroid gland. If the condition occurs secondary to kidney disease, however, it is more difficult to treat. In this case, administration of vitamin D and reduction of phosphorous (source of the body’s phosphate) intake can sometimes be helpful.
Hypoparathyroid myopathy
Symptoms: This type of endocrine myopathy is caused by underproduction of PTH from the parathyroid gland or alternatively, unresponsiveness of organs to PTH. Although it is not common, people with low parathyroid activity sometimes report mild muscle weakness. They may also exhibit low levels of calcium in the blood, which can lead to involuntary muscle contractions (known as muscle tetany).
Cause: Underactivity of the parathyroid gland or unresponsiveness to PTH can be a hereditary condition. In other cases, it may occur following surgical removal of the thyroid gland or due to dietary problems such as magnesium deficiency.
Management: If this condition is suspected, it can be confirmed by measuring the levels of calcium and magnesium in the blood. The myopathy that sometimes results from underactive parathyroid function can be alleviated by restoring normal calcium and magnesium levels using medication.
Adrenal gland myopathies
The adrenal glands are located on top of the kidneys. These glands produce a number of important hormones, including cortisol, aldosterone and adrenaline. The adrenal hormones help regulate metabolism, blood pressure, and the body’s response to stress. Function of the adrenal glands is under tight regulation; for example, release of cortisol is controlled by another critical hormone, adrenocorticotropic hormone (ACTH) produced by the pituitary gland at the base of the brain. An abnormal increase or decrease in cortisol levels that leads to muscle dysfunction can occur in several ways, including: iatrogenic Cushing syndrome, endogenous Cushing disease, and Addison disease (adrenal insufficiency).
Iatrogenic Cushing syndrome
Symptoms: This condition is caused by overactive cortisol function in response to steroid treatment. People with this condition often exhibit proximal muscle weakness and atrophy. Some concomitantly experience other conditions associated with muscle damage, such as sepsis, diabetes, acidosis, chronic obstructive pulmonary disease, or cancer, which can also be associated with abnormal adrenal hormone levels.
Cause: Synthetic steroids are often prescribed to treat autoimmune or inflammatory conditions. These steroids act like cortisol in the body, leading to overactive cortisol function.
Management: If a steroid-induced myopathy is suspected, muscle biopsy can sometimes be useful in differentiating this condition from other types of inflammatory myopathy. Steroid-induced myopathy can be treated by safely reducing the steroid dose over time to the lowest possible dose.
Endogenous Cushing disease
Symptoms: This condition is related to an overproduction of ACTH by the pituitary glands. People with Cushing’s disease typically experience proximal muscle dysfunction, ranging from myalgias (pain) to severe muscle weakness and atrophy.
Cause: In Cushing disease, overproduction of ACTH occurs as a result of a pituitary adenoma, a noncancerous tumor in the pituitary gland.
Management: Myopathy caused by endogenous Cushing disease can be treated by removing the overactive pituitary or adrenal tissue, thereby restoring normal hormone levels.
Addison disease (adrenal insufficiency)
Symptoms: This condition is related to underproduction of cortisol by the adrenal glands. People with this condition often exhibit generalized muscle weakness and fatigue.
Cause: The exact cause of Addison disease is not known, but it may result from an autoimmune condition that damages the adrenal glands.
Management: Addison disease can be life-threatening, but it is treatable. Treatment involves lifelong therapy to replace the missing cortisol with a synthetic version of the hormone.
How to prevent endocrine myopathies
In many cases, a healthy lifestyle and healthy behaviors can help delay the onset, minimize symptoms, or even prevent, endocrine myopathies. Some suggestions include:
- Regular check-ups to promote early detection and management
- Healthy diet to prevent nutritional deficiencies
- Regular physical activity to help maintain hormonal balance and promote muscle health
- Managing stress effectively to prevent stress-induced hormonal imbalances
- Avoiding harmful substances and toxins that may disrupt the endocrine system
- Adhering to recommended medical treatment plans to manage hormone imbalances and prevent development of myopathy
- Seeking genetic counseling if there is a family history of endocrine disorders or myopathy
Where to learn more about endocrine myopathies
It is important to note that this is not an exhaustive description of the endocrine myopathies. Additional endocrine disruptions may lead to muscle dysfunction, and additional symptoms may be present depending on the condition involved. While the endocrine myopathies are mostly treatable, the approach will differ based on the type and severity of the condition. Treatment plans are typically individualized to meet the needs of the affected person. People experiencing symptoms should reach out to their doctor for an evaluation and treatment recommendations.
For more information about the signs and symptoms of the endocrine myopathies, as well an overview of diagnosis, prognosis, and care management concerns, an in-depth review can be found from Rodolico, et al.
MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about endocrine myopathies, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
Next Steps and Useful Resources
- For more information about the Endocrine Myopathies, an in-depth review can be found here.
- For more information about the signs and symptoms of the endocrine myopathies, as well an overview of diagnosis, prognosis, and care management concerns, an in-depth review can be found from Rodolico, et al.
- MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about SELENON-related myopathy, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.