Simply Stated: Updates in LAMA2 Muscular Dystrophy
By Sujatha Gurunathan | Tuesday, February 20, 2024
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
LAMA2-related muscular dystrophy (LAMA2-RD) is a rare neuromuscular condition characterized by proximal (close to the body center), axial (head and trunk), and facial weakness, elevated creatine kinase (CK), central and peripheral nervous system involvement, and respiratory insufficiency. LAMA2-RD is a spectrum disorder that is generally divided into two main phenotypes: the more severe, early-onset form of congenital muscular dystrophy, often referred to as MDC1A and the milder, later-onset form of LAMA2-RD, often referred to as limb-girdle muscular dystrophy-23 (LGMDR23). A recent study using data from public, genetic databases estimated the worldwide birth prevalence of LAMA2-RD to be 8.3 cases per million people.
Symptoms of LAMA2-RD
The presentation of LAMA2-RD can be highly variable, depending on where a person’s condition falls on the disease spectrum.
The more severe phenotype of LAMA2-RD, MDC1A, begins at birth or within the first six months of life. MDC1A is often characterized as follows:
| Neuromuscular symptoms |
|
| Feeding/Gastrointestinal symptoms |
|
| Respiratory symptoms |
|
| Cognitive symptoms |
|
The disease phenotype known as later-onset LAMA2-RD or LGMDR23 is milder than MDC1A. People with LGMDR23 often begin experiencing symptoms during childhood, which may first be noticed in delayed motor milestones. Unlike MDC1A, affected individuals with the milder LGMDR23 achieve and maintain independent ambulation well into adulthood. Symptoms of LGMDR23 include the following:
| Neuromuscular symptoms |
|
| Cognitive symptoms |
|
For more information about the signs and symptoms of the LAMA2-RD, as well an overview of diagnosis, prognosis, and care management concerns, an in-depth review can be found from
Cause of LAMA2-RD
LAMA2-RD is caused by recessive mutations in the laminin alpha-2 (LAMA2) gene which encodes production of a subunit of the protein laminin-211, also known as merosin, and serves as an anchor between the muscle cell’s interior components and the extracellular matrix (ECM). Pathogenic mutations partially or fully inhibit the production of merosin, impacting the structure and function of muscle. Genetic changes that cause LAMA2-RD are inherited in an autosomal recessive pattern, which means that two copies of the defective gene (one from each parent) are required to cause the disease.
Diagnosis of LAMA2-RD
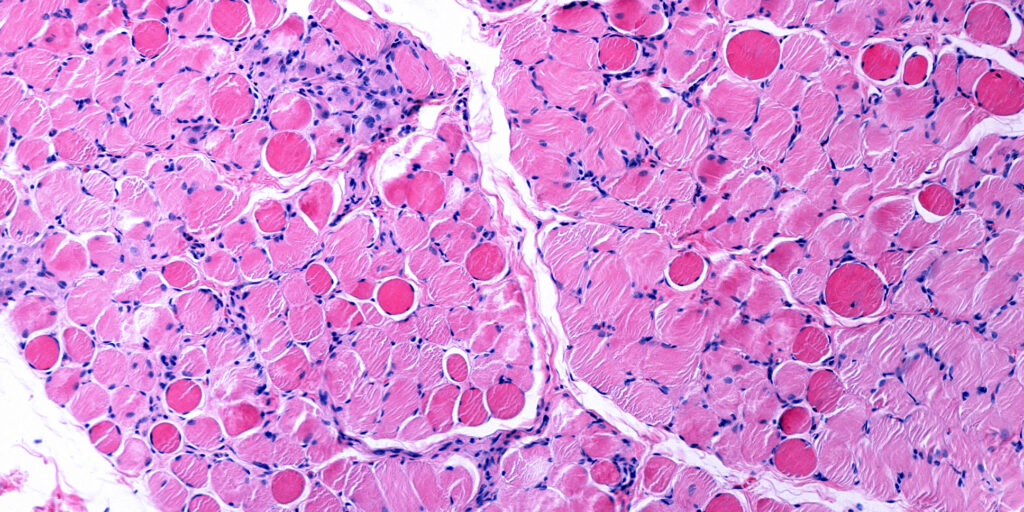
LAMA2-RD is typically diagnosed by genetic testing following clinical examination by a neuromuscular specialist. In some cases, testing may only successfully identify one copy of the mutation, but combined with clinical presentation, white matter changes on MRI, and sometimes skin or muscle biopsy can confirm a diagnosis of LAMA2-RD.
Management of LAMA2-RD
While there are currently no approved treatments for LAMA2-RD, proactive surveillance and care are critical to managing symptoms and disease progression, avoiding severe illness or hospitalization, and improving the affected individual’s overall health and quality of life. This includes multidisciplinary care by specialists in neurology, pulmonary medicine, nutrition, orthopedics, occupational, physical and speech therapy, as well as potentially other specialties (e.g., cardiology, ophthalmology). It is vitally important to begin breathing function surveillance by the age of 5 years old (if not earlier), which includes baseline pulmonary function testing and sleep study, with regular follow-ups to detect early signs of breathing decline. Close monitoring of feeding and nutrition with the potential for early intervention is also critical to overall health.
Evolving research and treatment landscape
While the current standard of care is proactive symptom management, research advances and the promise of therapeutic development on the horizon offer hope for people living with LAMA2-RD. Understanding of the genetic causes of LAMA2-RD is guiding preclinical development of new treatment strategies. For example, researchers are studying the therapeutic effects of increasing laminin levels as a way to counteract the effects of merosin-deficiency in cell and animal models. Some notable researchers to watch in the LAMA2-RD space include Dr. Avnika Ruparelia, Dr. Dean Burkin, Dr. Francesco Muntoni, Dr. Madeleine Durbeej, Dr. Nicol Voermans, Dr. A. Reghan Foley, Dr. Dwi Kemaldewi, Dr. Marc Güell, and Dr. Markus Rüegg, among others.
Observational studies and patient registry opportunities are also ongoing to better understand the disease course of LAMA2-RD and identify outcome measures that may be used for future clinical trials. One registry that is currently enrolling affected individuals is:
To learn more about research and clinical study opportunities in LAMA2-RD, visit clinicaltrials.gov and search for “LAMA2 muscular dystrophy” in the condition or disease field.
MDA’s work to further cutting-edge LAMA2-RD research
MDA is committed to furthering research in and therapeutic development for LAMA2-RD, and has funded more than $1.35 million in research grants since 2015. Recent MDA grants in LAMA2-RD include:
Linker-based gene therapy of LAMA2-related muscular dystrophy using AAVMYO (2022-2025)
Markus Ruegg, University of Basel
Dr. Ruegg’s laboratory has designed two artificial linker proteins that both bind to laminin-alpha 4. Muscle specific expression of both linkers in LAMA2-RD mice resulted in profound and long-lasting normalization of muscle histology, size, and strength. The aim of the project is to optimize linker delivery by using a new viral vector that targets skeletal muscle. This will lay the groundwork for future clinical trials.
Laminin enhancing small molecule for congenital muscular dystrophy (2019-2023)
Dean Burkin, University of Nevada
Dr. Burkin’s team has identified an FDA-approved small molecule, called PLX4023, which acts to increase laminin-511 in muscle. In this study they aim to study the effectiveness of PLX4023 in slowing muscle disease progression in a mouse model of LAMA2-RD. Since this molecule is already FDA-approved, successful outcomes of this project may more rapidly translate this new laminin-enhancing therapy for the treatment of LAMA2-RD.
Interrogation of CRISPR/Cas9-mediated exon inclusion in MDC1A (2018-2021)
Dwi Kemaladewi, University of Pittsburgh
The overall goal of this project is to assess the therapeutic potential of the restoration of laminin-alpha 2 protein using CRISPR/Cas9 gene editing technology in skeletal muscles and peripheral nerves in a MDC1A mouse model. Successful completion of the proposed projects will provide the necessary preclinical data and comprehensive strategy to bring CRISPR/Cas9-mediated gene correction closer to clinical application.
Using zebrafish congenital muscular dystrophy models to find novel therapies (2015-2018)
Peter Currie, Monash University
The goal of this project is the identification of a zebrafish mutation in the laminin-alpha 2 gene which is mutated in the most common form of congenital muscular dystrophy (CMD). Dr. Currie’s laboratory has used this zebrafish model to make observations on the mechanisms by why muscle cells die when they lack laminin-alpha 2 protein. New methods have been developed to screen drugs that prevent the onset and progression of muscle wasting in this zebrafish model. Potentially effective compounds could form the basis for the development of drugs to treat LAMA2-RD.
Together, these and other ongoing studies will help researchers to better understand LAMA2-RD, identify targets for therapeutic intervention, and test potential therapies. They will lay the groundwork for future clinical trials, improving prospects for better disease management for people living with the various forms of LAMA2-RD.
MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about LAMA2 muscular dystrophy, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
Other organizations serving the LAMA2-RD community include:
Cure CMD curecmd.org
Struggle Against Muscular Dystrophy (UK) helpsam.info
ImpulsaT (Spain) impulsat.org
LAMA2 France lama2.fr
Stichting Voor Sara (Netherlands) voorsara.nl
Olivia Bloomfield Foundation oliviabloomfieldfoundation.org
CMD Turkey cmdtr.com
AFM Telethon
Muscular Dystrophy UK
Muscular Dystrophy Canada
Next Steps and Useful Resources
- For more information about the signs and symptoms of Limb-Girdle Muscular Dystrophy, as well an overview of diagnosis and treatment concerns, an in-depth review can be found here.
- To learn more about research and clinical study opportunities, visit clinicaltrials.gov and search for “LAMA2 muscular dystrophy” in the condition or disease field.
- MDA’s Resource Center provides support, guidance, and resources for patients and families, including information, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Clinical Trials, Healthcare, Simply Stated
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




