Innovative Research: Spotlight on MDA Research Grant Recipients
By Larry Luxner | Friday, December 20, 2024
Since its founding 75 years ago, the Muscular Dystrophy Association has funded over $1 billion in neuromuscular disease research leading to life-saving treatments. This year, the MDA granted nearly $5.5 million in funding for 21 new projects, including the following two:
Neuromesodermal defects in SMA
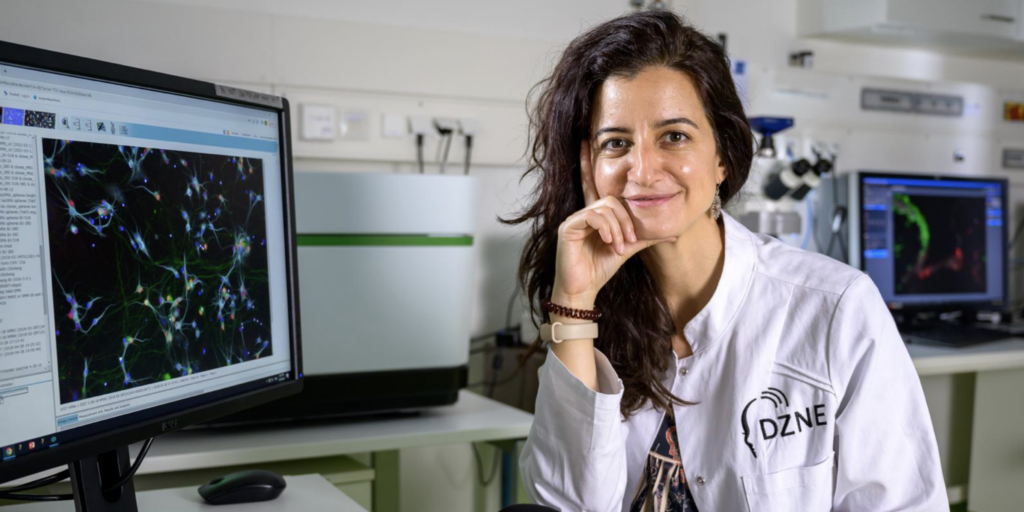
Natalia Rodríguez-Muela, PhD, of the German Center for Neurodegenerative Diseases (DZNE), is studying early neuromesodermal defects in SMA.
Natalia Rodríguez-Muela, PhD, of the German Center for Neurodegenerative Diseases (DZNE) in Dresden, has been awarded a $300,000 MDA grant to study the early neuromesodermal defects that are precursors to spinal muscular atrophy (SMA), a degenerative disorder whose most severe type can affect lifespan.
To date, the U.S. Food & Drug Administration has approved three therapies for SMA: nusinersen (Spinraza®), an injectable medication that won FDA approval in 2016; the gene therapy onasemnogene abeparvovec-xioi (Zolgensma®), which won FDA approval in 2019; and an oral therapy, risdiplam (Evrysdi®), approved in 2020.
“Although in many cases these treatments have drastically improved the disease prognosis, none of them represents a cure, even if administered soon after birth,” says Dr. Rodríguez-Muela, who is originally from Spain.
She adds: “There’s a diversity of responses to the treatment, so not all patients respond equally positively.”
The vast majority of current SMA research — like that for most neurodegenerative diseases, she argued — is postnatal and focuses on understanding how the motor neuron and the muscle cells degenerate to find ways to delay disease progression while ignoring the potential contribution of a developmental aspect to the pathology.
“In severe cases, the disease starts in utero. We already know this happens from mouse cells, our human organoids and scarce but solid data from postmortem fetal-infantile SMA tissues,” she says. “We believe that when levels of SMN protein are very reduced, early spinal cord development is altered. If we can understand the signaling pathway responsible for this, we could come up with approaches to correct it.”
What Dr. Rodríguez-Muela and her team hope to learn is whether early developmental defects constitute the basis of the pathology affecting motor neurons and muscle cells in severe forms of SMA. She also seeks to discover what causes those abnormalities during embryo development, then combine therapies with available SMN-increasing ones. For that, she’ll use complex patient-derived 3D in vitro human spinal cord organoid, as well as a commonly used mouse model, of SMA.
Gene repair therapy for limb-girdle muscular dystrophy

Charles P. Emerson Jr, PhD, and Scot A. Wolfe, PhD, are collaborating on an MDA-funded research project on limb-girdle muscular dystrophy (LGMD) at UMass Chan Medical School in Worcester, Mass.
Scot A. Wolfe, PhD, and Charles P. Emerson Jr., PhD, are collaborating on limb-girdle muscular dystrophy (LGMD) research at UMass Chan Medical School in Worcester, Massachusetts.
LGMD is an umbrella term that defines several rare disease types of muscular dystrophy that cause muscle weakness in the shoulders, upper arms, hips, and upper legs. This $300,000 MDA grant targets R7, a particular subtype of LGMD that affects fewer than one in a million people.
As Dr. Wolfe explains, “LGMD R7 is associated with mutations in the TCAP gene encoding for telethonin that interacts with titin in the sarcomeric Z-disk. Loss of telethonin leads to degeneration of muscles around the shoulder and core area. Patients slowly lose their ability to walk, require a wheelchair for mobility, and can have respiratory and cardiac challenges that can shorten their life span.”
There’s currently no cure for LGMD R7, nor even therapeutics to effectively treat the disease. Wolf and Emerson’s project combines stem cell, nanoparticle, mouse model, and genome editing technologies in translational studies to develop a corrective gene repair therapy, as well as establishing a platform to correct other gene mutations that cause the diversity of LGMD and other muscular dystrophies.
“The gene editing approach we’re using is called prime editing. What that allows you to do is precisely write any sequence you want into the genome,” Dr. Wolfe says. “It differs from base editors, which allow you to change a single base pair, and nucleases, which break the double strand of DNA and are typically imprecisely repaired. So, you could think about a prime editor like a word processor for the genome — you go into the text and delete a word, add a word, correct a misspelled word — whereas these other genome editing technologies are more limited.”
Dr. Wolfe said his team has been studying a common mutation in the TCAP gene since 2018.
“Originally, we were working on using nucleases for gene repair. We’ve done some testing of that in vivo and can show that we can turn TCAP back on, restoring protein expression,” he says. “Once we get prime editing optimized for correcting our target mutation in TCAP for R7, we’ll be able to apply the system to most other mutations by reprogramming the prime editor to provide a general approach for gene correction in myotubes and satellite cells.”
Conclusion
For 75 years, MDA has been at the forefront of groundbreaking research, advancing our understanding of neuromuscular diseases and bringing treatments and improving care for to countless individuals and families. Through innovative projects like Dr. Rodríguez-Muela’s study of developmental defects in SMA, and Dr. Wolfe and Dr. Emerson’s gene repair therapy for LGMD, MDA continues to push the boundaries of science.
These efforts are more than just medical milestones; they represent the dedication to improving lives and building a future with better treatments—and, ultimately, cures—within reach. To date, there are more than 25 drugs approved to treat neuromuscular disease, almost all of which benefited from direct or indirect MDA funding. The profound impact of the MDA’s work underscores the importance of ongoing investment in research and the collective power of science and collaboration to create meaningful change.
Next Steps and Useful Resources
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.