Help! Solutions Needed for Finding In-home Caregivers
By Myrna Traylor | Friday, May 3, 2024
For individuals living with neuromuscular diseases and their families, the search for reliable in-home caregivers is a constant and pressing challenge. Families face a sensitive balance between care needs and available support, and often, the scales are tipped against them due to factors in our healthcare system.
People with neuromuscular diseases and their families are reporting real and troubling experiences as they grapple with caregiver shortages, highlighting the dire need for effective solutions and advocacy at local, state, and federal levels.
What is in-home caregiving, and why is it hard to find?
In-home caregiving is a broad term for a variety of paid support services in the home. Home healthcare or skilled nursing care involves clinical services in an individual’s home provided by a professional, such as a nurse or physical or occupational therapist. These providers are often called home health aides.
“By contrast, home care or in-home personal care is non-medical and involves helping with things like activities of daily living — bathing, grooming, restroom assistance, meal preparation, light housekeeping, or transportation, no matter what condition the person has,” explains Lakelyn Eichenberger, PhD, a gerontologist and Caregiving Advocate at Home Instead. These caregivers are often called personal care attendants (PCAs).
The type of in-home services and caregivers that an individual uses is determined by need and, sometimes, by the agency providing caregivers.
The current caregiver shortage is caused by multiple factors. To name a few:
- A demographic shift, with the growing number of seniors requiring care, has increased the demand for home health aides.
- The perception of caregiving as “low-status” work, coupled with the marginalization of older adults and people with disabilities, makes it challenging to attract new workers to the caregiving profession.
- Insurance limitations serve as another significant barrier to securing necessary care. Many insurance policies, including those offered through Medicaid, have stringent eligibility criteria and coverage limitations that fail to meet the comprehensive needs of individuals requiring home and community-based services (HCBS). This gap often forces people with disabilities and older adults into more restrictive living settings, limiting independence and quality of life.

Sumukha Terakanambi
Stories of struggle
Sumukha Terakanambi, 25, was diagnosed with Duchenne muscular dystrophy (DMD) when he was 4 years old. He recently completed a master’s degree in public policy and hopes to work on the issue of support for families like his.
“Right now, I’m a contractor with a state agency that is like a disability advisory council in Minnesota,” he says. Sumukha recounts how, during the years when he was pursuing his master’s degree, he relied on family and friends to fill in the gaps left by the shortage of in-home caregivers provided through a Minnesota program called PCA Choice. Fortunately, that program will pay whomever Sumukha designates as his caregiver, including family or friends. He also uses In-Home Support Services (IHSS), another state-run program, to get personal care at home and while he is out in the community. “They can help with daily tasks — such as getting my water bottle out of my bag, setting me up for classes, preparing my food, helping me go to the restroom — but they cannot help with transfers,” he says.

Daniele Johnson and her son
Those needing in-home care that goes beyond daily tasks are often the hardest hit by the current situation. Indiana resident Daniele Johnson lost the home healthcare that helped her care for her 4-year-old son, Anthony Wade, who is living with zero-type spinal muscular atrophy (SMA). He requires constant monitoring to ensure he doesn’t pull out his ventilator trach or feeding tube. “We don’t get in-home nursing care through Medicaid; they stopped that in 2021,” Danielle says. “They said that because I wasn’t disabled and I wasn’t working at the time, we didn’t need a nurse, but I couldn’t go get a job because Medicaid denied the prior authorization for a nurse.”
Family caregivers are also struggling to find the support they need. Cori Tharp is the primary caregiver for her 17-year-old son, Nicholas, who lives with DMD. Cori has been trying to arrange occasional respite care in the evenings. However, the Tharps’ insurance offers extremely limited coverage for respite care — only four to six visits over the lifetime of the individual. In addition, she has struggled to find a home care service provider that offers respite care for minors.
Advocating for policy change

Cori Tharp
MDA is supporting legislative efforts to improve the situation for individuals and families who need non-medical in-home caregiving. Joel Cartner, MDA’s Director of Access Policy, outlined some bills that are moving through Congress that could help if enacted.
“The HCBS Access Act authored by Senator Bob Casey attempts to make complicated home and community-based services an entitlement similar to Medicare,” Joel says. “It’s a broad bill, but the entitlement piece would make permanent the appropriations for what’s called the Money Follows the Person program.”
Money Follows the Person (MFP) is a pot of federal money that states can use to help those with disabilities and older adults transition from inpatient settings to home and community-based settings. The MFP program seeks to do this by supplying funding directly to states, granting them the flexibility to invest in things like hiring and training staff, creating funds for home modifications, and forming partnerships with other state entities (housing agencies, health and aging agencies, transition specialists, etc.).
A related bill, the HCBS Relief Act, supplies temporary additional funding for HCBS services, including support for bolstering the number of professional caregivers available throughout the country. “That workforce pool is just so small,” Joel says. “Waiting lists for those services are incredibly long, so the bill works to improve training, recruitment, retention, and pay for people to provide the services.”
The urgency of this issue calls for continued dialogue, innovative thinking, and relentless advocacy. Contact your Congressional representative and senators and voice your support for the bills mentioned above. We invite you to join the conversation and be a part of the change that so many families desperately need.
Next Steps and Useful Resources
- Learn more in the MDA Guide for Caregivers
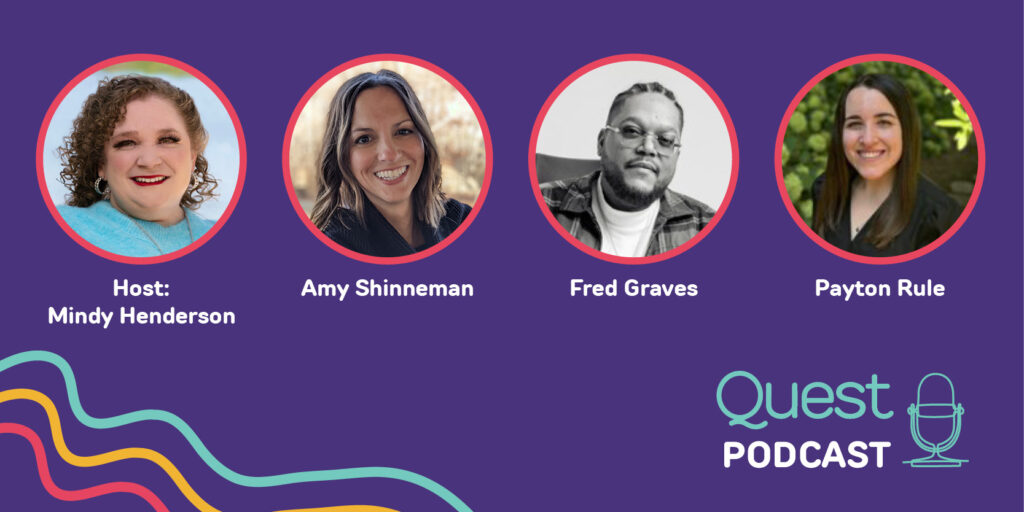
- Watch MDA Advocacy Institute Presents: Access to Care in the Home.
- Make a difference by becoming an advocate.
- To find caregiving resources in your area, contact the MDA Resource Center at 833-ASK-MDA1 or ResourceCenter@mdausa.org.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Caregiving, Featured Content, Personal Care Attendants
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.