Simply Stated: Research Updates in Congenital Muscular Dystrophy (CMD)
By Sujatha Gurunathan | Wednesday, October 26, 2022
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
Congenital muscular dystrophy (CMD) refers to a group of genetic muscle diseases that become apparent within the first two years after birth. CMDs belong to the larger group of disorders known as muscular dystrophies, which are characterized by weakness and degeneration of the voluntary muscles in the body that control intentional movements. Between different muscular dystrophies, the muscles affected, age of onset, disease severity and inheritance pattern can vary greatly. The exact incidence and prevalence of CMD is unknown, however, it is estimated that muscular dystrophies in general affect approximately 250,000 people in the United States.
Symptoms of CMD
People with CMD typically begin experiencing symptoms at or near birth. Most CMDs progress slowly over a long period of time. There are dozens of recognized subtypes of CMD, however, and symptoms, severity, and progression of disease can vary greatly by disease subtype. In general, CMD is characterized by decreased muscle tone (hypotonia), progressive muscle weakness and degeneration (atrophy), abnormal locking of joints (contractures), spinal rigidity, and delays in reaching motor milestones such as rolling over, sitting up, or standing without assistance. In some cases, potentially life-threatening complications such as feeding difficulties and breathing issues can develop. Rare forms of CMD may cause structural brain defects and affect intellectual ability.
Overview of CMD Subtypes
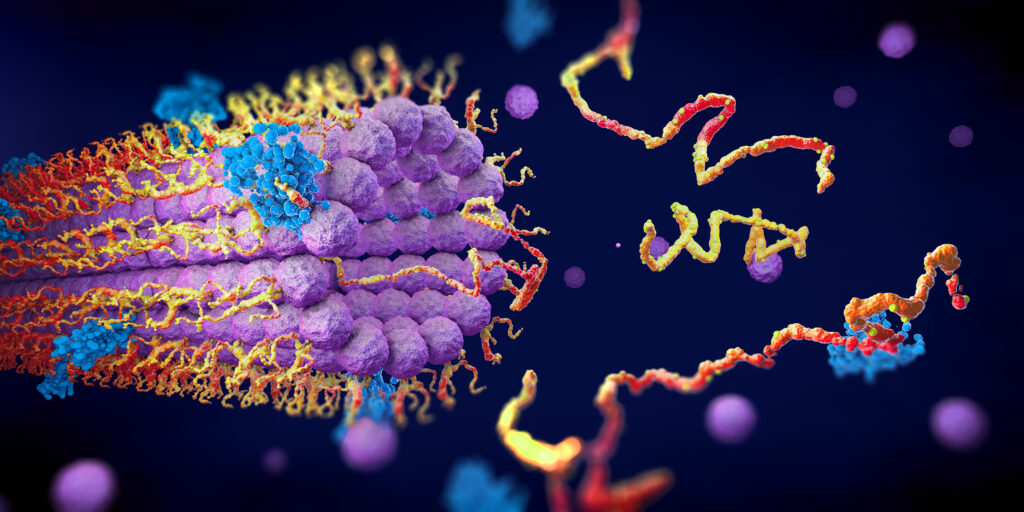
CMD is caused by genetic mutations that affect proteins necessary for the proper structure and function of muscles and sometimes for the eyes and/or brain. In most cases, CMD-causing defects disrupt the interaction between the muscle extracellular matrix (ECM), the complex that surrounds and supports muscle cells, and the muscle cell membrane (sarcolemma). As the genetic defects underlying CMD subtypes are identified, the understanding and classification of these diseases is rapidly changing. Many known CMD subtypes can be grouped by the type of genetic defects that cause disease. The following table presents some of the major known subtypes of CMD, but does not represent a complete list.
| Categories | Major Subtypes | Genetic Defects |
|
Laminin alpha 2 (LAMA2)-related (merosin deficient) CMD |
|
Defects in the ECM protein merosin |
|
Collagen VI–related muscular dystrophy |
|
Defects in an ECM protein (collagen VI) that helps anchor muscle, skin, cartilage, etc. tissues to the ECM |
| α-dystroglycanopathies |
|
Defects in proteins that help attach or bind (glycosylate) sugar molecules to dystroglycan, a protein in the sarcolemma of muscle cells |
| Laminopathy |
|
Defects in proteins found in the membrane (envelope) of the cell’s nucleus |
| Selenoprotein N1 (SEPN1)-related myopathy |
|
Defects in selenoprotein N1 protein, which protects cells against damage caused by free radical molecules |
Additional forms of CMD exist that are very rare or have not yet been linked to a specific genetic defect. For more information about the signs and symptoms of CMD, as well an explanation of the genetic underpinnings and subtype classifications of the disease, an in-depth overview can be found here.
Diagnosis of CMD
Symptoms of CMD overlap with those of other neuromuscular conditions, including the congenital myopathies and limb-girdle muscular dystrophies, making disease classification and clinical diagnosis challenging. Diagnosing a child with CMD may require a combination of the following testing modalities:
- Completing a family history and physical examination
- Electrodiagnostic testing (electromyography (EMG)/nerve conduction studies (NCS)) to assess muscle and nerve function
- Laboratory testing for muscle enzyme levels, presence of characteristic antibodies, and other clues to help diagnosis
- Imaging studies (ultrasound or magnetic resonance imaging (MRI)) to identify structural brain or other defects found in some CMD subtypes
- Biopsy to examine changes in muscle and nerve cells
- Genetic testing to identify gene abnormalities and confirm diagnosis of specific CMD subtypes
Consensus recommendations to help accurate diagnosis of CMD were published in 2014, though options for genetic testing have expanded in recent years.
Current management of CMD
While there is currently no cure for CMDs, multidisciplinary care can improve the overall health of people living with these diseases. Treatment plans are typically individualized to meet the needs of the affected person, and may include recommendations from a variety of specialists. Specific treatment options may include:
- Physical and occupational therapy to improve strength and prevent contractures
- Speech therapy to improve the ability to communicate
- Use of various assistive devices (e.g., canes, braces, walkers, wheelchairs) to improve walking (ambulation) and mobility
- Surgery to address skeletal abnormalities such as scoliosis
- Monitoring of the cardiac and respiratory systems to detect complications associated with some forms of CMD
- Use of assisted cough, noninvasive ventilation, or tracheostomy and mechanical ventilation to address respiratory insufficiency
- Overnight sleep studies to monitor breathing quality
- Use of gastrostomy tube to address feeding difficulties or severe failure to thrive
- Medical management of seizures
- Genetic counseling to understand diagnosis and help with family planning
- Social and emotional support for the entire family
Care recommendations to guide physicians in evidence-based treatment of people living with CMD were last developed by the International Committee on Standard of Care for Congenital Muscular Dystrophy
in November 2009. In the same year, a global partnership of patient advocacy groups, researchers, and clinicians, known as the CMD International Registry (CMDIR), was established to further development of new treatments for CMD. By participating in CMDIR, people with CMD provide critical data that is used for research to improve clinical care. They may also have chances to connect with other people with neuromuscular disease and to learn about clinical trials and other useful opportunities.
Evolving research and treatment landscape
While the standard of care is still symptom management, research advances and the promise of better therapeutics on the horizon offer hope for people living with CMD. Researchers have identified many of the gene defects that cause various forms of CMD. These discoveries have led to improved diagnosis and are guiding the development of new treatment strategies. Small molecule and gene manipulation/replacement technologies have been approved by the US Food and Drug Administration (FDA) for neuromuscular conditions such as Duchenne muscular dystrophy and spinal muscular atrophy, and these advances have led to hope that similar treatments may be developed for CMD.
While there are currently no clinical trials enrolling for CMD therapeutic candidates, there are some natural history studies underway that aim to better understand the disease course of CMD and identify outcome measures that may be used for future clinical trials. Examples include:
- The Natural History of Patients with Mutations in SEPN1 (SELENON) or LAMA2 (Radboud University Medical Center)
- Congenital Muscle Disease Study of Patient and Family Reported Medical Information (CMDPROS) (Cure CMD)
- Global FKRP Registry (Newcastle University)
- Clinical Trial Readiness for the Dystroglycanopathies (University of Iowa)
MDA’s work to further cutting-edge CMD research
Currently, disease-modifying small molecule and gene therapy strategies are being evaluated in pre-clinical studies for CMD. MDA is supporting several such efforts including:
Small molecules
Dr. Dean Burkin (University of Nevada, Reno), $300,000 MDA grant: “Laminin enhancing small molecule for congenital muscular dystrophy”
Gene therapy
Dr. Markus Ruegg (University of Basel), $300,000 MDA grant: “Linker-based gene therapy of LAMA2-related muscular dystrophy using AAVMYO”
In addition, MDA has funded several grants this year centered on understanding CMD and exploring disease-causing mutations. About 50% of all people with CMD lack a genetic diagnosis, necessitating the definition of biological pathways that contribute to CMD. Such foundational studies may facilitate development of new subtype-specific diagnostic testing, and potentially future therapies. Since its inception, MDA has invested more than $38 million in CMD research, with nearly $3 million spent on CMD-specific research grants in the last five years (2018-2022).
Next Steps and Useful Resources
- MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about congenital muscular dystrophy, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
- For more information about the signs and symptoms of Congenital Muscular Dystrophy, as well an explanation of the causes of disease, an in-depth overview can be found here.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.