Updates on LGMD2I/R9
By Myrna Traylor | Monday, February 12, 2024

Katherine Mathews, MD
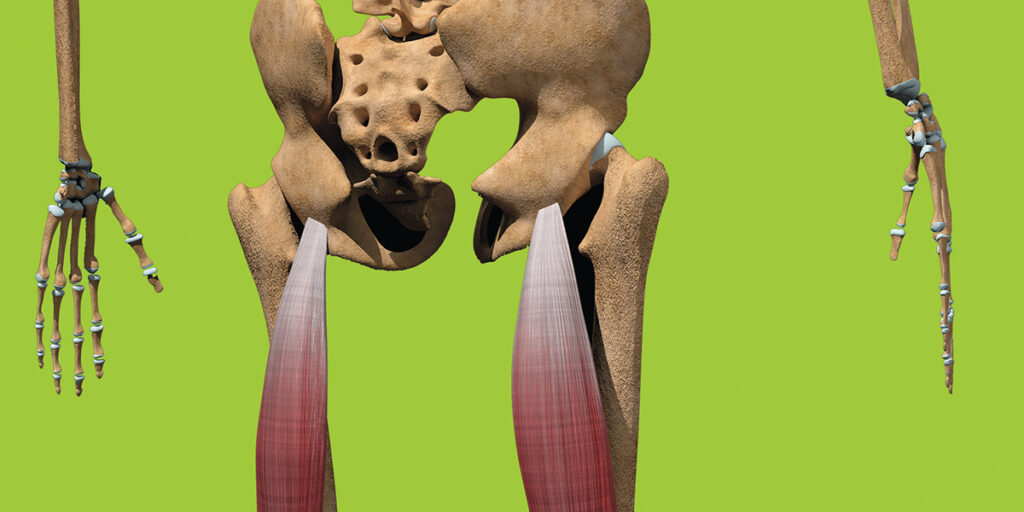
Limb-girdle muscular dystrophies (LGMD) include a diverse group of disorders with many subtypes. LGMD usually causes weakness in muscles around the hips and shoulders. The subtype LGMD2I/R9 (also called LGMD2I or LGMDR9) is the subject of some promising research.
To better understand LGMD2I/R9, we spoke with Katherine Mathews, MD, professor of pediatrics and neurology at the University of Iowa Carver College of Medicine. Dr. Mathews began her career as a pediatric neurologist and pursued a fellowship in genetics, focusing her early work on facioscapulohumeral muscular dystrophy (FSHD), for which she received funding from MDA. She later expanded her research interests to include other types of muscular dystrophy. For nearly 20 years, she has directed an NIH-funded natural history study to learn more about LGMD2I/R9 and related muscular dystrophies (dystroglycanopathies) as part of the University of Iowa’s Wellstone Muscular Dystrophy Specialized Research Center.
What is LGMD2I/R9?
LGMD2I/R9 is a type of limb-girdle muscular dystrophy that is inherited in an autosomal recessive pattern. Autosomal recessive means both copies of a gene inherited from both parents have a variation (mutation) that leads to disease. People with only one abnormal copy of the gene (from either parent) are healthy (carriers). LGMD2I/R9 is caused by two abnormal copies of the fukutin-related protein (FKRP) gene.
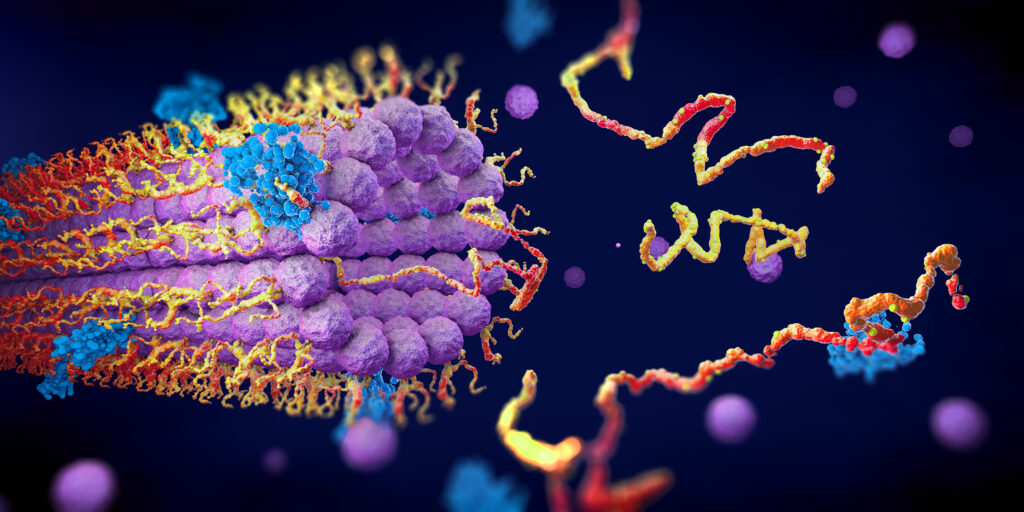
The FKRP gene is the “recipe” for fukutin-related protein, one of several enzymes required to put a chain of special sugars (called matriglycan) onto the protein alpha-dystroglycan. These sugar molecules help to bind the muscle membrane to a fibrous layer (extracellular matrix, or ECM) just outside the cell, providing stability to the muscle cell membrane. If fukutin-related protein isn’t working correctly, this connection to the extracellular matrix is weakened, and the muscle membrane is prone to breakdown. Ultimately, the muscle cell can die and be replaced by fat and scar tissue.
When is it typically diagnosed?
Like all forms of LGMD, there’s a wide age range in the onset and rate of progression. It can be diagnosed in young childhood or as late as middle adulthood. The diagnosis is suggested by weakness and often calf hypertrophy (enlargement). The muscle enzyme test, which measures creatine kinase (CK) levels in the blood, typically shows marked elevation. The diagnosis is confirmed by genetic testing.
What are the early signs and symptoms of LGMD2I/R9?
The most common symptom is muscle weakness or fatigue involving the hips, upper legs, or shoulders, typically first noticed during everyday activities like running or climbing stairs. Children with LGMD2I/R9 may present with intermittent severe weakness associated with a viral illness. They typically recover normal strength after they recover from the viral illness, but persisting laboratory abnormalities are a clue that they have muscular dystrophy.
People with a milder form of the disease may notice after vigorous exercise that their urine turns brown or tea-colored due to the breakdown of muscle cells, which releases iron-containing myoglobin that is excreted in the urine. This can be the first evidence of LGMD2I/R9. Another way people are diagnosed is through abnormal “liver enzyme” tests (such as AST and ALT) identified through blood work. Although they are called “liver tests,” these enzymes are also released from diseased muscle, so they are elevated in people with LGMD2I/R9.
What is the progression of the disease, and how is it managed?
LGMD2I/R9 results in progressive muscle weakness that worsens over time. The rate of progression depends on the person’s genetics, the type of FKRP gene mutation, and probably genetic background. Some FKRP gene mutations are known to be associated with less rapid progression.
An important part of management is monitoring the heart, as the heart muscle is also affected by abnormal fukutin-related protein activity. Heart monitoring is done by doing an echocardiogram (ECG), cardiac magnetic resonance imaging (MRI), or a combination of these tests every one to three years, depending on the individual situation, as guided by one’s neuromuscular doctor or cardiologist.
The muscles used for breathing can also be affected, so that’s another thing that needs to be monitored, using breathing tests (pulmonary function testing) or sleep studies. Some people need assistance with generating an effective cough or need breathing support at night.
Some people will need a wheelchair as early as their teens, while others won’t need a wheelchair until late adulthood.
Are there any treatments approved or being studied for LGMD2I/R9?
There are medicines to treat heart dysfunction, but there is not yet an approved medication specifically for LGMD2I/R9.
There are several clinical trials either in progress or in preparation. They revolve around two major approaches to therapy. One possible approach is gene replacement. The healthy gene can be put into a delivery system (currently through modified viruses). The modified virus carrying the FKRP gene is injected into the bloodstream. The new FKRP gene can turn on in the muscle. There are still questions about this approach. We don’t know the best “dose” of FKRP gene, as too much could be harmful and too little might not be effective. The infusion of the large number of virus particles used for gene delivery also has risks, including dysfunction of the heart, liver, clotting system, and kidneys.
Another approach being studied to treat LGMD2I/R9 is to try to make the existing fukutin-related protein work harder. We know that everybody who has LGMD2I/R9 has some fukutin-related protein activity because a complete absence is incompatible with life. Therefore, introducing a lot of one of the building blocks for the matriglycan sugar chain into the body might increase the amount of matriglycan on alpha-dystroglycan by driving fukutin-related protein to do more of what it normally does. This is predicted to increase its matriglycan binding to the ECM, making the muscle membrane less prone to damage and thus slowing the disease progression.
What is the origin of LGMD2I/R9?
Many genetic diseases have been found through mutations that arose in a population hundreds of years ago and have now spread throughout the world. These are called founder mutations. This particular gene, FKRP, has several founder mutations found in populations around the world. In the United States, almost everybody with LGMD2I/R9 has at least one copy of a Scandinavian founder mutation (c.826C>A) believed to have occurred at the time of the Vikings. People who have Scandinavian heritage are more likely to be carriers for this FKRP mutation. It’s not uncommon for people with LGMD2I/R9 to have two copies of this common founder mutation (one from each parent). Other people might have one copy of the founder mutation and one copy of a different mutation. People with two copies of that founder mutation tend to have a more slowly progressive course than people with other genetic patterns.
Myrna Traylor is a writer for Quest Media.
Next Steps and Useful Resources
- Browse our Diseases A-Z library of disease-specific content.
- Read more of the Quest Spotlight series on rare diseases.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Drug Development, Featured Content, Research, Spotlight
TYPE: Featured Article
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.