Five Questions with SMA Researcher Stephen Meriney
By Jeanene Swanson | Thursday, August 29, 2019
Stephen Meriney, PhD, professor of Neuroscience and Psychiatry at the University of Pittsburgh, was awarded an MDA research grant totaling $302,587 over three years to develop a combinatorial drug approach to discover possible therapeutics for spinal muscular atrophy (SMA). His work is focused on testing a novel calcium channel agonist (an agonist produces the same reaction as the molecule that usually binds the receptor) to boost motor neuron signal strength. He will also study combining this drug with the current antisense oligonucleotide (ASO) therapy for SMA.

SMA is caused by a mutated or missing survival motor neuron 1 gene (SMN1) that prevents the body from making enough survival motor neuron protein (SMN), ultimately leading to the loss of motor neurons, muscle weakness, and paralysis seen in SMA. SMA is the leading genetic cause of infant death. In December 2016, the US Food and Drug Administration (FDA) approved Spinraza, the first disease-modifying therapy to treat SMA in all patients. In May 2019, the FDA approved Zolgensma for the treatment of pediatric SMA patients, the first gene-replacement therapy for a neuromuscular disease.
Please describe your current research.
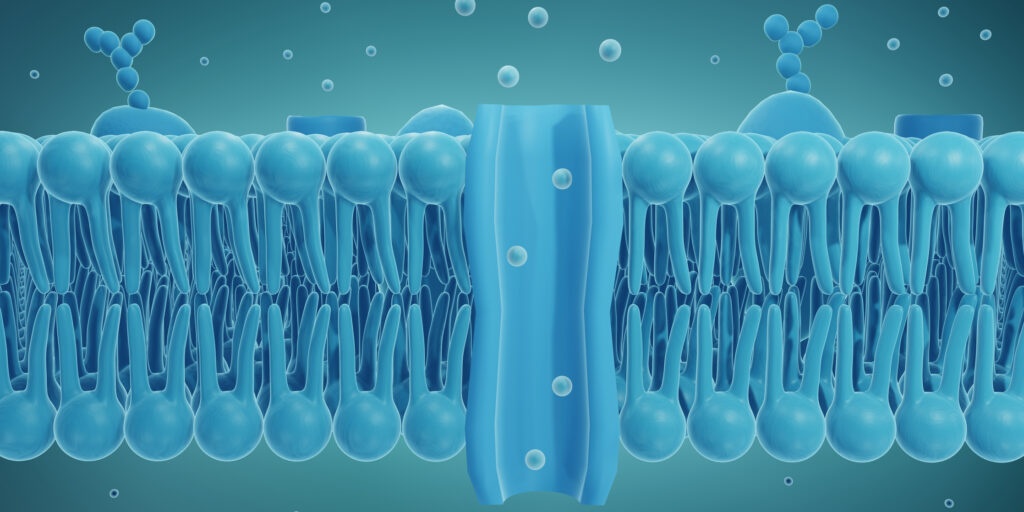
SMA is the leading genetic cause of premature death in children. SMA patients gradually succumb to muscle paralysis as a result of massive motor neuron degeneration. Patients with severe and intermediate forms of SMA experience lifelong physical disability and markedly shorter lifespans, with death as soon as one year (in severe patients). In December 2016, the FDA approved the first and only treatment for SMA, which utilizes intrathecally-administered ASOs upon SMA diagnosis. ASOs increase SMN protein expression and strongly improve motor function and lifespan in patients, but if mouse models are any indication, there are lingering deficits in neuromuscular strength. Treated SMA model mice have improved motor function and longer lifespans, though they remain weaker than healthy littermates. This is likely because ASO therapy occurs well after the first deficits are established, and central administration of ASO treatment may have reduced access to the peripheral neuromuscular synapses. Without treatment, low levels of SMN produce severe neuromuscular defects that result in up to 50% depression in neurotransmission in SMA model mice. Deficits include reduced calcium channel expression and clustering and fewer neurotransmitter release sites in neuromuscular junctions. These deficits contribute to reduced calcium entry into motor nerve terminals. Because neurotransmission is a calcium-triggered process, these reductions in calcium channels and calcium entry likely explain transmission deficits in SMA model systems.
We hypothesize that defective calcium entry underlies reduced neurotransmission in SMA neuromuscular synapses, and that ASO treatment incompletely rescues reduced neurotransmission. This lingering dysfunction ultimately leads to muscular weakness, which precedes motor neuron degeneration. Therefore, an SMN-independent approach that directly targets neuromuscular function by increasing neurotransmission would complement current therapy.
We propose to investigate a combination of ASOs (to prolong motor neuron degeneration and overall survival) plus a calcium channel agonist combined with a potassium channel blocker (to increase neurotransmission). We will evaluate these treatments by measuring calcium entry using fluorescent calcium imaging, neurotransmitter release using electrophysiology, and motor function using strength assays.
What is the focus of your research in SMA, and why is it important?
My focus has always been based on rational drug design. In other words, I try to understand the cellular and molecular details underlying the disease first, and use that information to guide a search for a new therapy. In the case of SMA, my laboratory defined the specific deficits at the neuromuscular junction that lingered after gene therapy was used to treat the underlying loss of the SMA protein. Then, we focused on trying to strengthen the neuromuscular synapse as an add-on therapy.
In the wake of the excitement surrounding the success of gene therapies to treat SMA, there was the realization that patients would need adjunct or add-on therapies to treat lingering deficits. This is critically important to assist patients in returning to normal activities of daily living.
What inspired you to study SMA?
While an MDA postdoctoral fellow at the Jerry Lewis Neuromuscular Research Center at the University of California, Los Angeles, in the late 1980s, I studied neuromuscular synapses with Dr. Alan Grinnell. During that time, I was exposed to a variety of neuromuscular diseases and became inspired to develop a research program to study the pathophysiology and potential treatment approaches to these diseases.
What is the expected outcome of your research?
Following completion of the proposed work, we expect to evaluate a candidate therapy for lingering neuromuscular weakness deficits in an SMA model mouse. These studies will form an important part of a pre-clinical package that we plan to generate to move candidate therapies forward for eventual testing in humans.
How will your research lead to treatments and cures?
This project will directly test a novel treatment to address neuromuscular weakness in SMA patients. This treatment is not a cure but rather a symptomatic approach to increase acetylcholine release from neuromuscular synapses.
Why is it important that MDA continue to fund research in SMA?
Although SMA can now be treated using newly approved gene therapy, there are still important needs for this patient population. Most importantly, there are many patients living with SMA who were born before the gene therapy was available, and for these patients, the gene therapy may only prevent further motor neuron degeneration. Therefore, these patients in particular will benefit from alternative treatment options. These new alternative treatment options can only be developed following extensive basic and pre-clinical research that is essential for their discovery and testing. Without MDA funding support, it would be very difficult for these studies to be conducted.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.