Simply Stated: Elevated Enzymes
By Sharon Hesterlee, Evrim Atas, and Angela Lek | Thursday, April 6, 2023
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
Elevated enzymes are a frequently encountered problem in general medical practice, but their meaning often isn’t so simple to discern. When they’re found with a neuromuscular disease, the situation can get complicated.
What’s an enzyme?
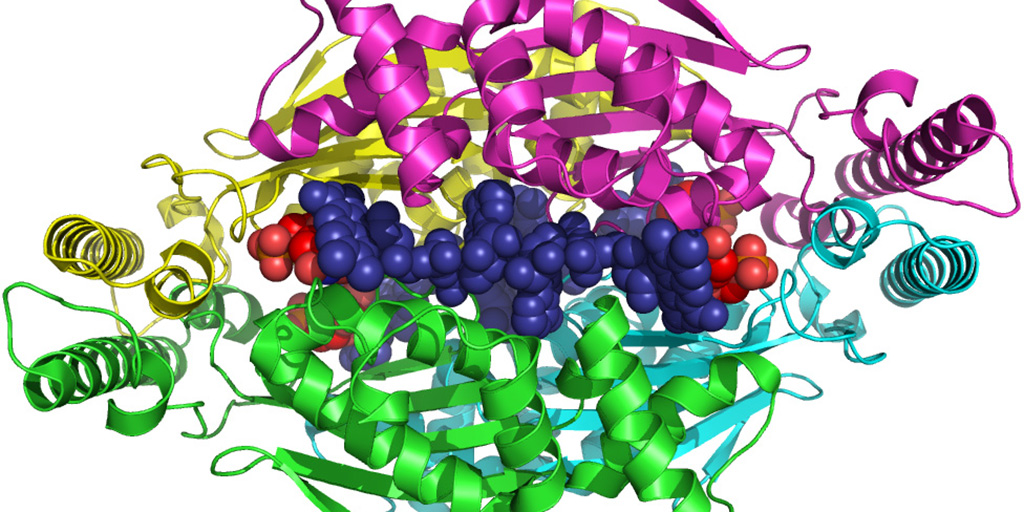
There are thousands of enzymes in the cells in our bodies, where they act as catalysts for all the chemical reactions that take place in these cells. Without them, these reactions either wouldn’t occur or would be too slow for the cells’ needs.
Many enzymes are normally present in the blood and can be measured there. When cells are damaged by disease or injury, large amounts of these leak out, causing blood tests to show that enzymes are elevated above normal. (You can roughly compare this situation to a car that’s leaking oil. Leaks in many parts of the engine can have the same result: oil all over your driveway.)
Where did it come from?
Measuring enzymes is only a clue to a possible diagnosis or problem, not a diagnosis in itself. An elevated enzyme level on a screening test should prompt a physician to look further into which areas of the body may be leaking enzymes into the blood, just as a good mechanic looks for the source of a car’s oil leak. (In either case, finding the source is only the first step. The next steps are finding out why the leak has occurred and attempting to fix it.)
Two enzymes often measured on routine tests are known as ALT (alanine transaminase) and AST (aspartate transaminase). ALT is found in the liver, heart, muscles and kidneys. AST is in the liver, heart, muscles, kidneys, brain, pancreas, spleen and lungs. ALT is also known as SGPT (serum glutamic-pyruvic transaminase), and AST is also called SGOT (serum glutamic-oxaloacetic transaminase).
In many neuromuscular disorders, muscle tissue is gradually damaged, either by an attack from the immune system (as in inflammatory myopathies), or by a genetic mutation inside the cells (as in the muscular dystrophies). When routine tests measuring ALT or AST are performed in people with neuromuscular disorders, these enzymes are often elevated in the blood, because the ALT and AST are leaking out of damaged muscles. But they can also leak out of other organs, particularly the liver.
Liver or muscle?
If a neuromuscular disorder hasn’t yet been diagnosed, a doctor may be misled into thinking that a damaged liver, not damaged muscles, is the source of the enzyme leak. In the general population, liver damage is more common than muscle damage, so this assumption isn’t too surprising.
The careful physician will, however, investigate further. An enzyme called GGT or gamma-GT (gamma-glutamyltransferase, also gamma-glutamyltranspeptidase) is found in the liver but not in the muscles. If it’s unclear whether the liver is damaged, a normal GGT level can help a doctor decide that it’s not, while a high GGT level would sway him or her toward thinking it is. (That’s far from the only test that can be done, but it’s an easy and relatively inexpensive one.)
CK (creatine kinase), also called CPK (creatine phosphokinase), is only found in the heart, skeletal muscles and brain. The MM form of CK is the type found in skeletal muscles, and it can be specifically measured when a doctor suspects a muscle problem. A normal CK level with elevated ALT and AST enzymes would sway a doctor toward thinking there’s a liver problem; a high CK with high ALT and AST levels suggests that something’s going on in the muscle.
So, doing additional enzyme tests after a general screen can help a doctor decide whether the high ALT and AST are more likely the result of liver or muscle damage.
Of course, there could be a problem in both liver and muscle. (Your 1982 Volvo could be leaking oil from both the oil pan and a gasket.) Some metabolic muscle disorders, such as acid maltase deficiency and debrancher enzyme deficiency, affect both tissues. And two diseases can occur in the same person.
What damages the liver?
A person at high risk for hepatitis or other liver damage, whether or not he or she has a neuromuscular disease, needs further attention focused on the liver, with the medical history and physical exam taken into account. Liver problems may occur in someone who’s had blood transfusions before 1990 (before modern hepatitis virus testing), taken drugs (prescription, over-the-counter or recreational) that are known to damage the liver, recently eaten potentially contaminated shellfish, had a history of malignancy or recently been stabbed in the abdomen — whether there’s a neuromuscular disease or not.
The medications riluzole, used to treat amyotrophic lateral sclerosis, and methotrexate, used to treat inflammatory myopathies and myasthenia gravis, are among the many drugs that have liver-damaging potential.
Most of the time, elevated ALT and AST levels in people with degenerating muscles don’t mean much, other than that these enzymes, along with CK, are leaking out of the muscles. (The high levels of enzymes do no harm in and of themselves.) But sometimes, depending on results of other tests and the person’s history, they can mean there’s trouble in the liver or even in another organ. That’s where medical detective work is needed.
Serum enzyme levels of CK, LDH, ALT and AST are the most widely measured enzymes in patients suspected of having a muscle disease. However, it should be noted that the deficiency of a specific enzyme can also be the underlying cause of a muscle disease. For instance, people with metabolic myopathies lack certain enzymes involved in providing energy that help muscles contract. The affected muscles can’t function normally leading to symptoms like progressive muscle weakness, exercise intolerance and even heart problems. Different forms of metabolic myopathies are distinguished by which enzyme is deficient or missing. Examples of diseases associated with reduced levels of specific enzymes include Pompe disease which is caused by acid maltase deficiency; and McArdle disease which is due to a lack of enzyme that assist in carbohydrate metabolism. For more information on enzyme-deficient metabolic myopathies see: (https://www.mda.org/disease/metabolic-myopathies/types)
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Next Steps and Useful Resources
- MDA’s Resource Center provides support, guidance, and resources for patients and families, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org
- For more information about the signs and symptoms of Metabolic Myopathies, as well an explanation of the causes of disease, an in-depth overview can be found here.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Healthcare, Simply Stated
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




