Simply Stated: Muscle Biopsy
By MDA Staff | Friday, February 23, 2024
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
A muscle biopsy is a surgical procedure in which one or more small pieces of muscle tissue are removed for microscopic examination and biochemical or genetic testing. The procedure, sometimes used in the diagnosis of a muscle disorder, is considered “minor” surgery and is usually performed under local anesthetic.
Muscle biopsy used to be more commonly used in the diagnosis of neuromuscular diseases, but the last decade has seen advances in the fields of imaging and genetic testing. These diagnostic methods are noninvasive and generally quite accurate. Muscle biopsy is being used less frequently as a first-line diagnostic test.
Now, in people with suspected inherited muscle disease, genetic testing is usually performed first. If genetic testing is inconclusive, muscle biopsy may be done to help clarify the results of genetic testing.
Muscle biopsy is still commonly used in diagnosing inflammatory and necrotizing myopathies.
Open or needle biopsy
There are two types of muscle biopsy. The open biopsy is the most common. It involves the removal of one or more small pieces of muscle tissue with sharp scissors.
The neuromuscular specialist selects a muscle, usually the biceps, deltoid, or quadriceps muscle, that should yield the most information about the disease. Usually, moderately affected muscles are chosen; the weakest muscles may already be too degraded for analysis. The procedure involves a 2-to-3-inch incision, which is then closed with stitches and may feel sore for a few days.
In a needle biopsy, a pea-sized muscle sample is collected with a large bore needle. Although this is less invasive than the open biopsy, the specimen collected is much smaller and may miss the diseased area in the muscle.
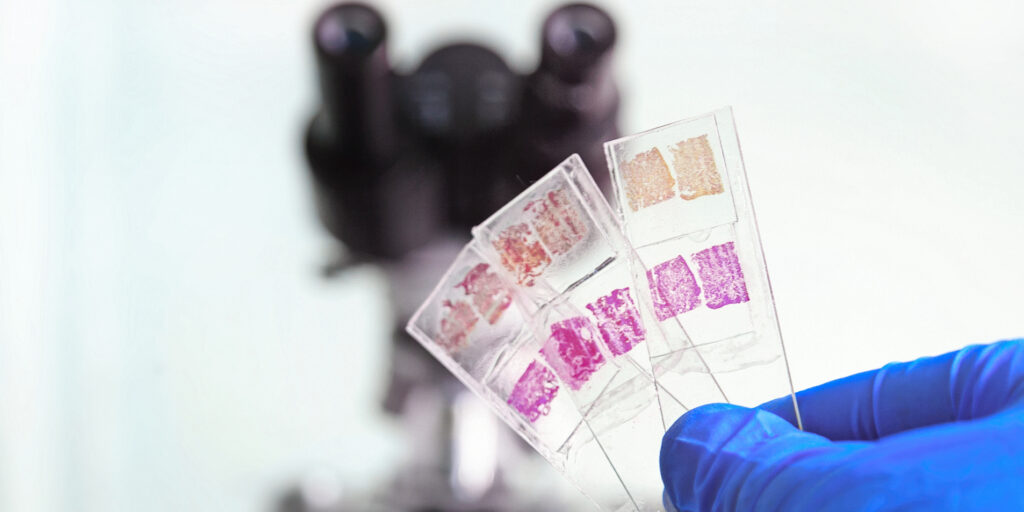
Analyzing the sample
When the muscle samples are sent to a laboratory for analysis, the technicians cut them into many thin sections for examination. Using different stains on different sections, the muscle pathologist looks at the tissue’s overall appearance, chemical activities in the tissue, and the presence or absence of critical proteins. The information these tests provide helps determine exactly what disease and what form of it the person has.
Types of analysis
Histology tests (histo means tissue) employ chemical stains to see the muscle’s overall appearance and the structure of the muscle cells. This analysis can yield information about muscle degeneration and regeneration, fiber type abnormalities, mitochondrial abnormalities, scar tissue, inflammation, and other clues to specific disorders.
Histochemistry uses stains to detect chemical activities in the cells, including the actions of specific enzymes and metabolic processes. A lab that performs only histology may miss important metabolic abnormalities.
Immunohistochemistry uses antibodies to detect the presence or absence of muscle proteins. This analysis can show whether the muscle fibers are missing dystrophin (indicating Duchenne or Becker muscular dystrophy), sarcoglycans (limb-girdle muscular dystrophy), merosin (congenital muscular dystrophy), or other proteins whose absence causes specific muscular dystrophies. Immunohistochemistry testing is not performed regularly because genetic testing generally detects these abnormalities.
The lab may also use electron microscopy to get very high magnification views of the muscle fiber structures, which can confirm structural abnormalities, like the presence of nemaline rods.
Finally, a DNA analysis can be performed on a muscle sample to detect a genetic mutation when genetic testing using a blood or spit sample is inconclusive. A muscle sample may be needed to detect some mitochondrial DNA mutations.
Depending on the lab, results may be available in as little as three days or as long as two weeks.
Saving samples
In some cases, multiple samples are taken to be used for different types of analysis and testing. Muscle tissue that is frozen and maintained properly is useful for many years. Some institutions keep these samples for a set number of years, and others keep them indefinitely. Frozen samples may be used for additional testing later or in research, with the individual’s consent.
Next Steps and Useful Resources
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Featured Content, Genetic Testing, Healthcare, Simply Stated
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




