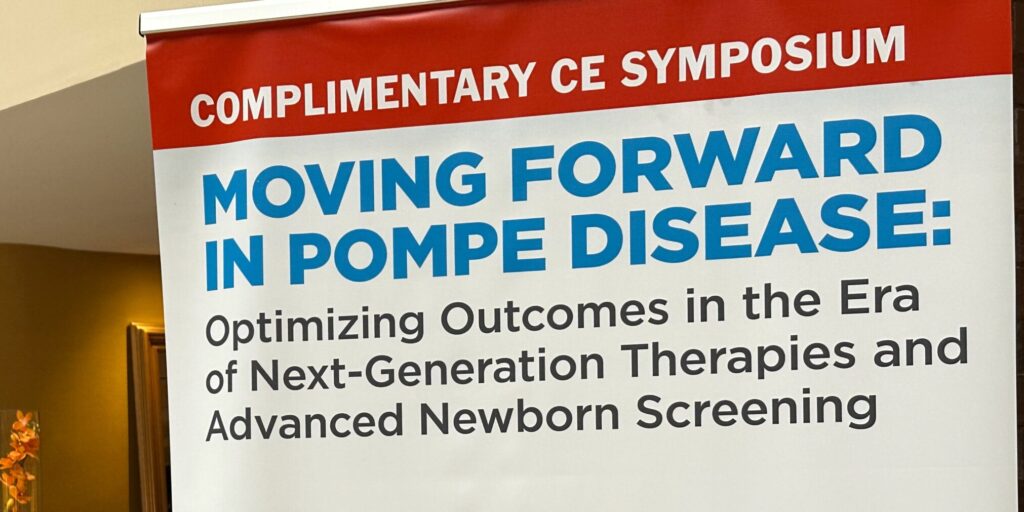
At MDA Conference, Pompe Disease Researchers Stressed Importance of Newborn Screening
By Larry Luxner | Friday, April 14, 2023
With 38 states now screening newborns for Pompe disease and therapies widely available to improve quality of life if it is diagnosed early enough, there’s no reason the 12 states not checking for Pompe shouldn’t add this disease to their screening panels.
That’s the overriding message from a Pompe disease symposium held on March 20, 2023, at the MDA Clinical & Scientific Conference in Dallas.
“This is something I have long advocated for and had nominated in 2008 to the Recommended Uniform Screening Panel [RUSP]. It finally got on the panel in 2015,” said Priya Kishnani, MD, MBBS, a pediatric medical genetics specialist at Duke University in Durham, North Carolina.
The RUSP is the national list of diseases recommended for screening. Newborn screening is a public health program that falls under the authority of the states, so the final decision on whether to test for a specific disease is up to each state.
Pompe disease, named after the Dutch pathologist who first described it in 1932, is also known as acid maltase deficiency or glycogen storage disease type II. Caused by a deficiency or lack of acid alpha-glucosidase (GAA) enzyme, its classic or early-onset form generally results in death by a patient’s first birthday if left untreated. Patients with late-onset Pompe disease (LOPD) can present from as early as the first few months of life to as late as the sixth decade. The differentiating feature from infantile-onset Pompe disease (IOPD) is the absence of cardiomyopathy in the first year of life.
Dr. Kishnani emphasized that early diagnosis of Pompe is critical. “For infantile Pompe, days matter — even a delay by a few days can impact the clinical outcome for these babies,” she said. For LOPD, which people often think of as an adult illness, early diagnosis also can make a difference. “From real-world data, it’s very clear that for many children with LOPD who are clinically identified, these kids have a huge diagnostic delay of up to 12 years,” she said.

Tracy Boggs, PT, NCS, is a board-certified specialist in neurologic physical therapy at Duke University. Photo Credit: Larry Luxner
More cases than previously thought
Before widespread newborn screening for Pompe, the disease was believed to affect 1 in 40,000 births. But researchers now say its prevalence ranges anywhere from 1 in 9,000 (in Missouri) to 1 in 20,000 (in Illinois, New York, and Michigan). Up to 2,000 gene variants are believed to exist.
“It’s very clear that there are way more cases than we thought, and that the majority of those are LOPD. These are the ones that were missed or have this huge diagnostic odyssey,” Dr. Kishnani said.
At present, three therapies have been approved by the US Food and Drug Administration (FDA) to treat Pompe disease. The first, alglucosidase alfa (Myozyme) won FDA approval in 2006 for IOPD. It was later marketed as Lumizyme for LOPD. Then in August 2021, the FDA granted accelerated marketing approval to avalglucosidase alfa (Nexviazyme) to treat patients 1 year of age or older living with LOPD.
Dr. Kishnani detailed the case study of a baby whose LOPD was detected through newborn screening. The infant had low muscle tone and gross motor delays, but Pompe probably would not have been suspected if it hadn’t been for the newborn screening.
“Nexviazyme was not available then, so we started her on standard-of-care alglucosidase alfa enzyme replacement therapy,” she said. “As we watched her, we recognized that she was improving. We started therapy at 11 months, and she’s now 5 years old and doing really well. You couldn’t distinguish her from any other typical child.”
Tracy Boggs, PT, NCS, a board-certified specialist in neurologic physical therapy who also works at Duke, has been treating patients with Pompe disease since 2011. She recommends exercise routines of moderate intensity that combine aerobic, strength, balance, and flexibility.
“I know that awareness [of Pompe] is increasing. People are talking about it,” said Boggs. She’s also noticed that diagnoses are becoming more accurate. “When I started seeing patients 12 years ago, I’d frequently have people who had been misdiagnosed for years with some other type of muscular dystrophy,” she said. “These days, that is less common.”

Paula Clemons, MD, is a neurologist and microbiology professor at the University of Pittsburgh. Photo credit: Larry Luxner
Therapy advances
Paula R. Clemens, MD, a neurologist and microbiology professor at the University of Pittsburgh, spoke about next-generation enzyme replacement therapies.
She said LOPD symptoms generally appear between the ages of 20 and 50, but these enzyme replacement therapies stabilize patients. “There is still continued slow decline, but it is a much lower decline in both respiratory function and physical function than in the untreated state,” she said.
She added that four companies — AskBio, Astellis, Audentes, and Spark — are pursuing gene therapies for Pompe. In addition, Maze Therapeutics is planning a new study of an oral substrate reduction therapy, designed to decrease levels of glycogen inside muscle cells. Dr. Clemens said she is “quite optimistic” about a major breakthrough in the next five to 10 years.
Next Steps and Useful Resources
- Read Simply Stated: Research Updates in Pompe Disease.
- Learn about efforts to improve the newborn screening program.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Drug Development, Featured Content, Gene Therapy, MDA Clinical and Scientific Conference, Research, Research Advances
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.