Guiding Treatment for Myotonic Dystrophy
By MDA Staff | Monday, July 15, 2019
Myotonic dystrophy (DM) is the most common form of muscular dystrophy in adults. This is a complex disease, affecting not just the muscles, but nearly every other organ system in the body. The signature manifestation is myotonia, an inability to consciously relax the muscles, coupled with progressive muscle weakness.
There are two types of DM, each caused by a different genetic mutation.
DM1 is the most common form, with three subtypes:
- Adult onset, also called “classical DM,” is the most common type, affecting about 75 percent of those with DM. It begins in adolescence or adulthood, typically with myotonia. Over time, the muscles throughout the body become weaker and other organs are affected.
- Juvenile onset begins between ages 1 and 10. It is characterized by cognitive and behavioral symptoms, including attention deficit disorder and anxiety, as well as muscle weakness and myotonia.
- Congenital onset begins at or before birth and features severe muscle weakness, cognitive impairment and other developmental abnormalities.
DM2, sometimes called proximal myotonic myopathy (PROMM), typically begins in adulthood and tends to be less severe than DM1.
Numerous medical conditions occur with both forms, including cardiovascular complications, gastrointestinal symptoms (in DM1), a higher risk of certain cancers, male infertility and low testosterone, high cholesterol and low blood pressure, and insulin resistance.
Quest turned to Tetsuo Ashizawa, M.D., a professor of neurology and director of the Neurosciences Research Program at Houston Methodist and Weill Cornell Medical College, and a leading expert in DM, for an update on treatment and efforts to find a cure for the disease. Most of what you’ll read here refers to DM1.
Can you explain the genetic component of DM?
DM1 results from a mutation in the DMPK gene and DM2 from a mutation in the CNBP gene.
The mutation in the DMPK gene leads to an expansion of a cytosine-thymine-guanine (CTG) trinucleotide repeat in the DNA. (Nucleotides are molecules that make up DNA and RNA.) Normally, we have up to 37 CTG repeats at this location. But most of those with DM have a much higher number of repeats, sometimes in the thousands. In DM1, the larger the repeat, the earlier the symptoms appear and the more severe they are. Also, the number of repeats in DM1 may increase with each generation. So while a grandparent may have few symptoms, a grandchild may have many. This is called “genetic anticipation.”
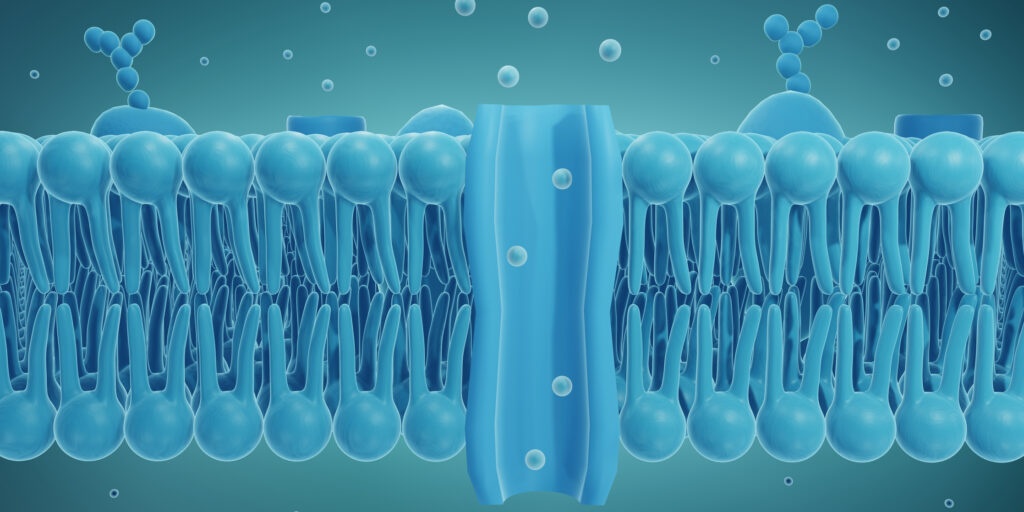
The mutated gene, in turn, produces an expanded version of messenger RNA, which is responsible for reading the DNA “code.” These RNA molecules become toxic and interfere with the production of other proteins, preventing normal cell functioning.
Is there any treatment for DM?
 We can treat the symptoms. There are some medications that can help improve myotonia and muscle pain (which primarily occurs in DM2).
We can treat the symptoms. There are some medications that can help improve myotonia and muscle pain (which primarily occurs in DM2).
People with DM may develop problems with arrhythmias, or irregular heartbeats, which can lead to heart failure and sudden death. Thus, people with DM often receive a pacemaker or defibrillator.
Exercise is a good idea. We used to think that DM muscles are fragile and break down easily, but it turns out that regular physical activity may prevent muscle atrophy. However, it is important that people with DM check with their doctor before beginning any exercise program.
Are there guidelines for diagnosing and treating DM?
The first-ever Consensus- Based Care Recommendations for Adults with Myotonic Dystrophy Type 1 were published last year. Currently, there are no evidence-based guidelines to establish a standard of care for patients with DM because the rigorous clinical studies needed to gather the necessary data have yet to be conducted. Thus, many patients report difficulty finding and accessing quality care and informed clinicians. The newly published recommendations are intended to help standardize and elevate care for people living with DM.
Where is the research on finding a cure for DM?
A better understanding of the disease is driving research into new targets for treatment, most directed at the toxic RNA. These include antisense oligonucleotides (ASOs). The ASO binds to the target RNA and destroys it, thus restoring function. While successful in animal models, the one human clinical trial so far didn’t show any clinically detectable therapeutic effects. Now researchers are working on a better delivery system for humans. If ASOs can be delivered to muscles and other organs, it may address many of the complications of the disease.
Another option is to use a genetic tool called CRISPR to remove the expanded DNA repeat from the gene itself. But that is 10 to 20 years down the road.
What can those with DM do today to help advance research?
They can enroll in a registry that helps recruit people for clinical studies. They also can participate in longitudinal natural history studies. Understanding the natural history of the disease is important for future clinical trials in order to track the efficacy of drugs and understand ethnic, gender and age-related differences in the disease. There are two registries: Myotonic Dystrophy Family Registry, managed by the Myotonic Dystrophy Foundation, and the Myotonic Dystrophy and Facioscapulohumeral Muscular Dystrophy Registry, run by the National Institute of Neurological Diseases and Stroke. People with DM can enroll in both.
They can also volunteer for clinical studies. There are numerous ongoing clinical trials investigating everything from drugs that target the disease itself to treatments for the complications and genetic studies to better understand how the disease manifests in families.
Find a Trial
Learn what to expect in a clinical trial and find out if there is a study you can enroll in at mda.org/research/clinical-trials.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.