What About My Disease? Why a New Treatment for One Neuromuscular Disease Is Good News for All
By Cheryl Alkon | Monday, February 27, 2023
Recent treatment advances for Duchenne muscular dystrophy (DMD) and spinal muscular atrophy (SMA) have generated a lot of excitement in the neuromuscular disease community. They’ve also led a lot of community members to ask, “What about my disease?”
News about advances for any neuromuscular disease is good news because new methods and treatments for these conditions pave the way for potential treatments for other neuromuscular diseases, even those considered ultra-rare.
The first step in treating genetic disorders

Peter Kang, MD, says growing knowledge of therapies used to treat DMD and SMA can be applied to other diseases.
In 2003, the Human Genome Project finished mapping all the genes in the human body. This ushered in a promising new era for treating genetic disorders. Identifying and understanding the genetic cause of a disease is a critical first step toward developing therapies that target the root cause of that disease.
At the forefront of this effort are gene replacement and oligonucleotide therapies. “These two molecular therapeutic approaches are rippling through numerous diseases,” says Peter Kang, MD, director of the Paul and Sheila Wellstone Muscular Dystrophy Center at the University of Minnesota. In particular, the US Food and Drug Administration (FDA) has approved four oligonucleotide therapies for DMD and one for SMA. One gene therapy is FDA-approved for SMA, with several in human clinical trials to treat diseases including limb-girdle muscular dystrophy (LGMD) and facioscapulohumeral muscular dystrophy (FSHD).
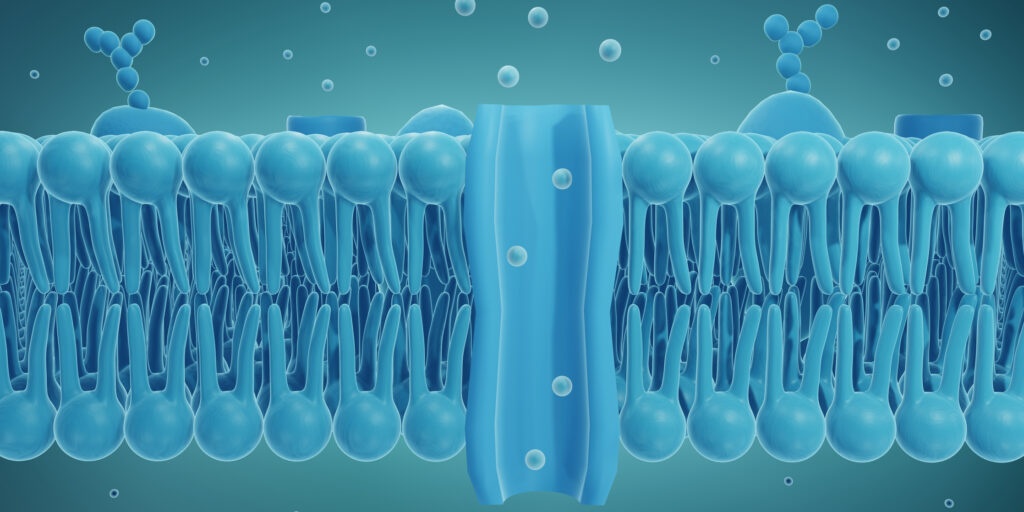
Oligonucleotides are short strands of DNA-like molecules that are injected into a person to alter the way genes are expressed and how cells make proteins.
Gene replacement therapy works by delivering a functional version of a gene into targeted cells in the body to replace a malfunctioning or non-functioning gene.
For kids with SMA type 1, Zolgensma — a gene replacement therapy — appears to stop the disease’s progression. “It has been revolutionary for babies with SMA,” says Alan Beggs, PhD, the Manton Professor of Pediatrics at Harvard Medical School and director of the Manton Center for Orphan Disease Research at Boston Children’s Hospital.
“Children who likely would not have survived their first year of life typically thrive and grow, with many eventually learning to stand and walk.”

Alan Beggs, PhD, is studying using the gene therapy method used to treat SMA for other diseases.
Promising research
Dr. Beggs currently is researching using gene therapy to transfer a missing protein to people with X-linked myotubular myopathy (XLMTM), an ultra-rare neuromuscular disease that occurs in 1 in 50,000 newborn males worldwide. Clinical trials are ongoing, and a paper describing the first studies is currently under review. “What was done for SMA and what’s being done here are parallel,” he says, noting that this is an example of a treatment method developed for one neuromuscular disease that can translate to another.
Michael Shy, MD, the Carver College of Medicine endowed chair of inherited neuropathies at the University of Iowa, is using animal models to study using antisense oligonucleotides (ASOs) or RNA interference (RNAi) to help people with Charcot-Marie-Tooth disease (CMT) or other hereditary motor sensory neuropathies, which cause damage in the peripheral nerves that send messages from the brain or spinal cord to the muscles. “The most common form of CMT is caused by increased amounts of a gene and its protein called peripheral myelin protein 22. ASOs and RNAi can decrease the levels of this gene and protein,” he says.
In addition, due to the success of the therapies already developed, many biotechnology companies are working on future human clinical trials for rare neuromuscular diseases.
Continuing to learn about rare diseases
Every preclinical study, human clinical trial, and FDA approval of an oligonucleotide or gene therapy teaches researchers lessons that help them refine subsequent studies.
“Our knowledge of these therapies and how they behave in various settings and different types of patients is becoming increasingly sophisticated, expediting their application to other categories of diseases,” Dr. Kang says.
From the researchers’ perspective, progress made for one neuromuscular disease is progress for all diseases.
“What we learn about SMA, we can apply to other diseases,” Dr. Beggs says. “For every disease, we are learning new things, and everything we learn will help us move faster for other diseases because we know to watch out for certain characteristics. I’m cautious but very excited for the future.”
Next Steps and Useful Resources
- Download MDA’s education sheet about Genetics and Neuromuscular Disease in English or Spanish.
- Read about gene therapy and how drug developers are listening to the neuromuscular disease community’s perspective on clinical trials.
- Learn about common inheritance patterns of genetic neuromuscular diseases.
- Register for the 2023 MDA Clinical & Scientific conference: mdaconference.org.
- Learn more about the Rare Disease Track and all of the tracks at the conference on the agenda here.
- Read about how MDA’s Kickstart program launched a pilot project to develop a gene therapy for an ultra-rare type of congenital myasthenic syndrome (CMS).
- Stay up to date on all of Quest’s content by subscribing to Quest Magazine and Newsletter: https://www.mda.org/quest/subscribe.
TAGS: Antisense Oligonucleotide, Clinical Trials, Drug Development, Featured Content, Gene Therapy, Innovation, Research
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.