What You Need to Know About Feeding Tubes and Nutrition
By Cheryl Alkon | Monday, July 10, 2023
For people diagnosed with amyotrophic lateral sclerosis (ALS) and other neuromuscular diseases that make it hard to eat, chew, or swallow, using a feeding tube helps them get the nutrition and hydration they need.
The feeding tube, known as a gastrostomy or gastric tube (g-tube), is implanted through a small incision in the stomach. A g-tube can be placed for nutrition, hydration, and/or medication administration.
A standard g-tube has 12 to 18 inches of tubing that extend out from the skin; once the body has healed from the surgical incision, it can be changed to a low-profile tube that lays flush with the abdomen, according to Shayne Robinson, MSRD, CSO CDN, a clinical dietician at New York-Presbyterian/Columbia University Irving Medical Center.
When is a feeding tube necessary?
A feeding tube may be needed when it becomes difficult to swallow food or liquid. Considerations include weight loss; whether fatigue limits the ability to cut, chew, and swallow food; and breathing ability. The individual’s preferences and readiness are also important.

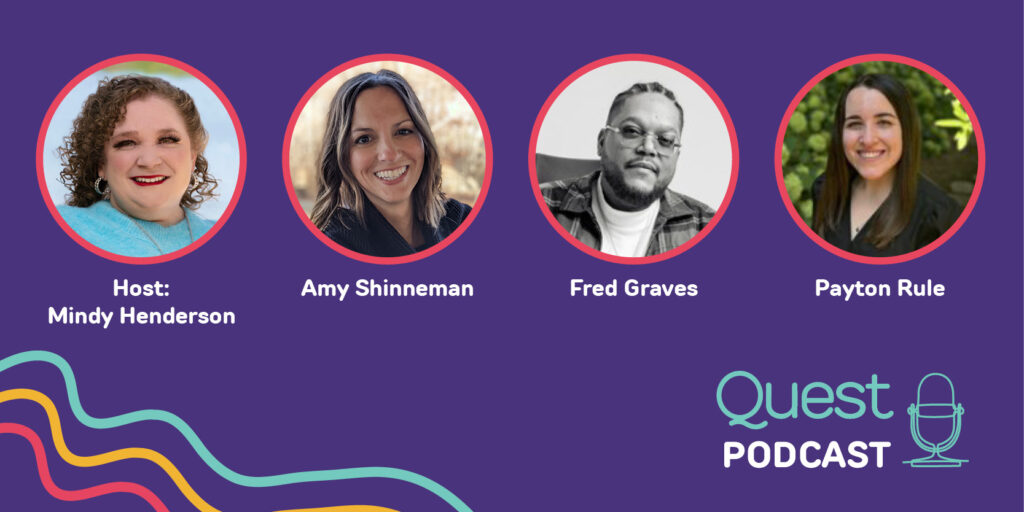
Julia Yasek, RN, FNP-BC, DNP, is a nurse practitioner who works with people with ALS.
Julia Yasek, RN, FNP-BC, DNP, is a nurse practitioner who works with people with ALS.
Photo credit: Columbia University Irving Medical Center
Some healthcare providers recommend having a g-tube placed before it is needed in the case of a progressive neuromuscular disease.
“Usually, it’s best to have a tube placed before a patient has trouble breathing while lying flat or when their vital capacity — how much air a person can exhale after taking a deep breath — is 50%, whichever occurs first,” says Julia Yasek, RN, FNP-BC, DNP, a nurse practitioner at the Eleanor and Lou Gehrig ALS Clinic at Columbia University.
Placing a feeding tube can be mildly uncomfortable at first; the individual may need pain management for the first few weeks after insertion. Once the site heals, the tube should not hurt at all. When using the tube, there can be discomfort if the nutrition or hydration is pushed through the tube too quickly or is too cold. “Slowing it down or warming it up can resolve this easily,” Julia says.
Feeding tube nutrition
It’s still possible to eat or drink by mouth if you have a g-tube, as long as it is safe to swallow and you have no medical restrictions to take anything by mouth. “Those who take a regular or modified diet often use a feeding tube for supplemental nutrition, hydration, or medication administration,” Julia says.
While people with g-tubes have the same nutritional needs as everyone else, they may have some special considerations because of their disease.
“People who tube feed should consult with a registered dietician for a regimen that is best for their medical condition,” Shayne says.
You can use blended foods or commercially prepared formulas with a g-tube. If you blend foods, Shayne recommends straining the blends to prevent clogging the tube.
Nutritionally complete formulas are available on Amazon or can be ordered directly from manufacturers. You may also order formula through a regular or specialty pharmacy. If a person depends entirely on tube feeding, their insurance may cover the formula.
Prices vary — a standard formula costs about $57 for a case of 24, and most people who don’t eat by mouth use four to six containers a day. “At six a day, you are looking at $14.25 a day for formula — less than a Sweetgreen salad,” Julia says.
How to feed with a g-tube
There are several ways to provide nutrition or hydration with a g-tube:
- Insert a syringe in the tube to deliver a serving of food or formula.
- Fill a feeding bag and elevate it to allow the food or formula to flow through the tube.
- Attach a feeding bag to a pump that provides continuous feeding over a period of time.
The most common methods used by adults with neuromuscular diseases are the syringe or elevated feeding bag, according to Julia.
To help hold the syringe or bag during feeding, Shayne recommends a product called the FreeArm that clamps to the side of a wheelchair, table, or bed. “It is like having an extra hand,” she says. Other people like using a stretchy fabric band to hold the tube in place during feeding.
Benefits of tube feeding
A g-tube tube “can allow a patient to lead a longer, more comfortable life in the face of a life-altering diagnosis,” Julia says.
One benefit is avoiding choking or aspiration episodes at meals, which can be scary for individuals and caregivers. Some of Julia’s patients tell her the g-tube helps them enjoy the social aspects of mealtime again because they don’t have to worry about finishing their plate or eating with impaired chewing and swallowing.
Ultimately, choosing a g-tube can improve quality of life, as well as provide good nutrition.
Next Steps and Useful Resources
- Read Who’s on Your MDA Care Team?: Dietitians and Nutritionists.
- Watch the Nutrition and Neuromuscular Disease MDA Engage webinar to learn more about healthy eating.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.