Simply Stated: Research Updates in Leigh Syndrome
By Sujatha Gurunathan | Wednesday, December 6, 2023
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
Leigh syndrome is a rare, neurodegenerative disorder caused by defects in the mitochondria, the energy-producing structures within our cells. This disorder often begins in infancy or early childhood and causes brain abnormalities that can cause developmental delays and a variety of debilitating symptoms. The exact prevalence of Leigh syndrome is not known because some cases receive alternative diagnoses or are classified broadly as mitochondrial disease. The National Library of Medicine reports an estimated incidence of the disease as 1 in 40,000 newborns.
Symptoms of Leigh syndrome
Many people with Leigh syndrome begin experiencing symptoms before 24 months of age, though late childhood and adult disease onset have also been reported. Leigh syndrome can progress rapidly and present with a diverse range of symptoms, which may include, but are not limited to:
- Impaired coordination (ataxia)
- Involuntary muscle movement (dystonia)
- Paralysis of the eye muscles (external ophthalmoplegia)
- Progressive neurodegeneration
- Seizures
- Stroke-like episodes
- Buildup of lactate in the body (lactic acidosis)
- Vomiting
- Generalized weakness
- Decreased muscle tone (hypotonia)
- Impaired breathing (respiratory) function
- Heart complications (e.g., cardiomyopathy, arrhythmias)
- Developmental delays
Currently, the prognosis for this disease is poor and the disease is typically fatal. Most children with Leigh syndrome do not survive past the age of 3 years old. For more information about the signs and symptoms of Leigh syndrome, as well as an explanation of the genetic underpinnings of the disease, in-depth overviews can be found from Bakare et al., 2021 and Rahman, 2023.
Cause of Leigh syndrome
Leigh syndrome was first described in 1951 by the British psychiatrist Denis Archibald Leigh as a complex and incurable neurodegenerative disease, with onset during infancy, called subacute necrotizing encephalomyelopathy (SNE). After decades of research, it is now known that Leigh syndrome belongs to a class of disorders known as mitochondrial disorders.
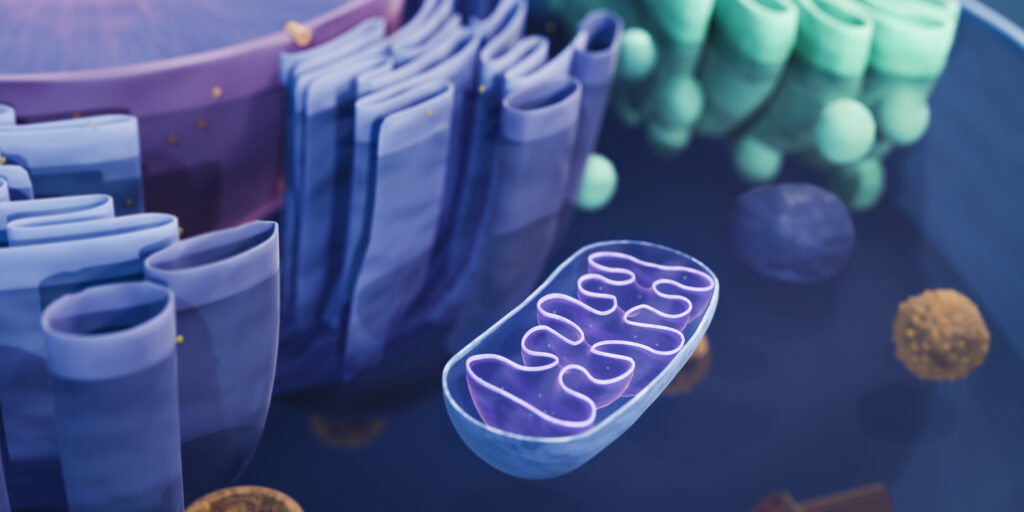
Mitochondrial disorders are caused by inherited mutations affecting the function of mitochondria, the energy-producing structures in our cells. As a result, these disorders typically impact organ systems with high energy requirements, such as the central nervous system (i.e., brain and spinal cord), heart, and skeletal muscles. Mutations that cause a mitochondrial disorder can occur in either mitochondrial DNA or nuclear DNA, leading to vastly different inheritance patterns. The diversity in disease-causing mutations results in conditions that have a wide range of clinical manifestations and functional impairments.
In the case of Leigh syndrome, researchers have identified defects in 16 mitochondrial genes and almost 100 nuclear genes that are thought to cause the condition. This is one of the reasons that clinical presentation may differ so drastically between different people with Leigh syndrome. In general, the mutations that cause Leigh syndrome affect the ability of the mitochondria to produce energy through a metabolic pathway known as oxidative phosphorylation. This can lead to impairments in a number of areas in the brain, including the brainstem, cerebellum, basal ganglia, thalamus, and oculomotor and cranial nerves, as well as the spinal cord, which in turn, can affect the control of motor movements.
Diagnosis of Leigh syndrome
Leigh syndrome can be difficult to diagnose; the symptoms can be variable and may be mistaken for other conditions. Brain visualization by magnetic resonance imaging (MRI) can be used to identify the characteristic brain lesions and tissue damage seen in people with Leigh syndrome and help with diagnosis. Brain imaging, combined with family history, clinical exams and laboratory testing (e.g., biochemical testing for mitochondrial enzyme levels, blood tests for enzymatic activity, muscle biopsy and histopathology to identify muscle changes, genetic testing for disease-causing gene variants, etc.) may be collectively used to establish a diagnosis of Leigh syndrome.
Current management of Leigh syndrome
There is currently no known cure or disease-modifying therapy for Leigh syndrome. However, some strategies may help ease symptoms and improve quality of life for people with the disease. Vitamins, including coenzyme Q10, L-carnitine, and thiamine (Vitamin B1) may be prescribed to help boost metabolism (the process of turning food into energy) and provide antioxidant effects. Oral sodium bicarbonate or sodium citrate is sometimes given to manage lactic acidosis. In some cases, diet modification may be beneficial. Given the variability of symptoms experienced by different people with Leigh syndrome, treatment plans are typically individualized to meet the needs of the affected person and may include recommendations from specialists such as neurologists, clinical geneticists, cardiologists, and/or nephrologists.
Evolving research and treatment landscape
Preclinical research using various model systems is helping to define the underlying defects that cause Leigh syndrome and other mitochondrial disorders and to investigate potential therapeutic candidates. A recent overview of ongoing preclinical research can be found in the review by Bakare et al., 2021.
The current approach to treatment of Leigh syndrome focuses on improving energy production while lowering lactate levels. One of the biggest challenges to developing new treatment options for Leigh syndrome is the variability of the disease. Some targeted development efforts are focusing on therapies to increase the number, function, and/or health of the mitochondria in the cells and tissues affected by Leigh syndrome.
Clinical research into new therapies for Leigh syndrome also presents hope for improved disease management. Examples of therapeutic candidates under investigation include:
EPI-743 (PTC Therapeutics) – EPI-743, also known as vatiquinone, is an antioxidant molecule and analog of coenzyme Q10 (an important molecule for mitochondrial energy production) that has been suggested to improve clinical outcomes in some cases of Leigh syndrome. EPI-743 is being studied in an active phase 2 clinical trial.
NV-354 (Abliva) – NV-354 is an engineered version of succinate, a natural compound in the body that can fuel mitochondrial energy production. In April 2023, NV354 was granted orphan drug designation (ODD) by the FDA based on its positive pre-clinical data, thereby facilitating its clinical development, and potentially expediting its future path to regulatory approval.
MNV-201 (Minovia) – MNV-201 is an innovative stem cell therapy that is designed to augment levels of healthy mitochondria in the body. The therapy remains in preclinical development for Leigh Syndrome but is undergoing testing in Phase I clinical studies for Pearson Syndrome, a similar fatal mitochondrial disorder that affects infants.
Observational studies and patient registries are also underway to collect data and use it to (1) better understand the genetic underpinnings and disease course of Leigh syndrome and (2) identify outcome measures that may be used for future clinical trials. Some studies/registries that are currently enrolling include, but are not limited to:
The International Registry for Leigh Syndrome (The University of Texas Health Science Center, Houston)
Tissue Sample Study for Mitochondrial Disorders (Columbia University)
North American Mitochondrial Disease Consortium Patient Registry and Biorepository (NAMDC) (Columbia University)
To learn more about clinical trial and research study opportunities in Leigh syndrome, visit clinicaltrials.gov and search for “Leigh syndrome” in the condition or disease field.
MDA’s work to further cutting-edge Leigh syndrome research
MDA is committed to furthering research in and therapeutic development for Leigh syndrome and has funded about 2.6 million in research grants since 2000. In 2023, MDA funded a new study by Dr. Antoni Barrientos at the University of Miami Miller School of Medicine, which investigates the role of aberrant folding of mitochondrial mRNA (genetic material that carries instructions for making mitochondrial proteins) as a propagating disease factor in Leigh Syndrome. Prior MDA funding supported research studies focused on uncovering novel molecular mechanisms underlying Leigh Syndrome and developing new cellular and animal models of the disease.
Together, these studies and those of other notable researchers will help to better define this rare disease and to identify new targets for therapeutic intervention. They will lay the groundwork for future clinical trials, thereby improving prospects of better disease management and survival for people with Leigh syndrome.
MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about Leigh syndrome, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org
Next Steps and Useful Resources
- Be A Light of Hope and Donate at MDA.org/HOLIDAY
- For more information about the signs and symptoms of Leigh Syndrome, as well an overview of diagnosis and treatment concerns, an in-depth review can be found here.
- To learn more about research and clinical study opportunities in PP, visit clinicaltrials.gov and search for “Leigh Syndrome” in the condition or disease field.
- MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about Leigh Syndrome, open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




