Simply Stated: Research Updates in Spinal-Bulbar Muscular Atrophy (SBMA)
By Sujatha Gurunathan | Tuesday, August 1, 2023
5 Second Summary
“Simply Stated” is a Quest column designed to explain some terms and basic facts about neuromuscular diseases.
Find more at Mdaquest.org/tag/simply-stated
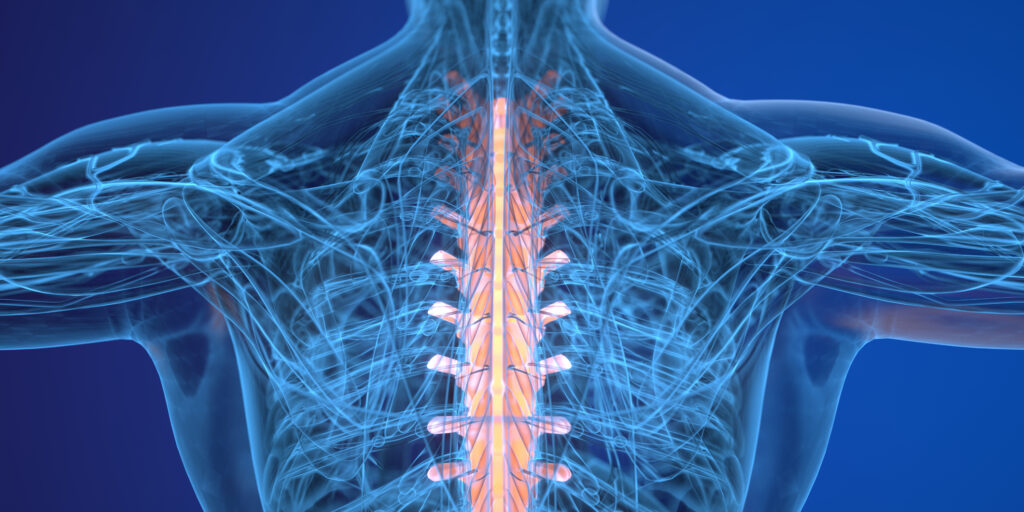
Spinal-bulbar muscular atrophy (SBMA) is a genetic disorder in which degeneration of lower motor neurons, the nerve cells that connect the spinal cord and brainstem to the muscles, causes slow, progressive weakness, atrophy (thinning or loss), and fasciculations (twitching) in muscles throughout the body. In many people, SBMA affects facial and swallowing muscles, as well as muscles in the arms and legs. The disease can also cause hormonal dysfunction related to the loss of testosterone activity. SBMA primarily affects adult males, with an estimated prevalence of about 1 in 300,000 men.
SBMA is sometimes called Kennedy disease, after William Kennedy, the physician who originally described the condition in 1968. It is also sometimes called bulbospinal muscular atrophy. The term “bulbar” is a reference to the bulblike structure in the lower part of the brain that contains nerve cells that control muscles in the face, mouth and throat.
Symptoms of SBMA
Men with SBMA typically begin experiencing symptoms between the ages of 30 to 50 years old, though the disease may appear earlier or later in some people. Early signs of SBMA are difficulty walking and a tendency to fall. Many affected people also experience muscle cramps. SBMA continues to progress very slowly, over the course of decades.
By one to two decades after symptom onset, most affected people will experience muscle weakness and atrophy in their arm and leg muscles, particularly in the muscles nearest the center of the body. They may notice twitching or cramping of their limb muscles, and many will have difficulty climbing stairs. About one-third of affected people will require a wheelchair 20 years after symptom onset.
Most people with SBMA eventually show dysfunction in their bulbar muscles, which results in difficulty with speaking and swallowing. In severe cases, affected people may be at risk for aspiration pneumonia, a lung infection caused by food or liquid entering the airways or lung, or for lung failure due to weakness of the bulbar and respiratory (breathing) muscles. These complications are uncommon, but can be life-threatening. Most people with SBMA, however, have a normal life expectancy.
SBMA can also cause hormonal issues in men with the disease. Men with SBMA sometimes develop enlarged breasts, known as gynecomastia, and may have reduced fertility and atrophy (shrinking) of the testicles. These symptoms are related to abnormal processing of male hormones, known as androgens, which include the hormone testosterone.
In the few women who have SBMA, the symptoms are usually mild. Female carriers of the flawed gene that causes SBMA sometimes develop muscle cramps and twitches, particularly as they get older (>60-70 years old).
For more information about the signs and symptoms of SBMA, a detailed clinical overview of SBMA can be found here.
Cause of SBMA
SBMA is caused by a genetic defect in the androgen receptor (AR) gene found on the X chromosome. The AR gene contains a repeated sequence of DNA known as a CAG triplet repeat. Most people have fewer than 34 CAG repeats in their AR gene, leading to production of normal androgen receptor proteins. People with SBMA, however, have an abnormal expansion of the number of CAG repeats in their AR gene, with more than 38 CAG repeats present. Scientifically, this change is referred to as a “trinucleotide repeat expansion.” The normal function of the androgen receptor is to help cells process androgens, including testosterone. Abnormal expansions in the AR gene causes production of defective androgen receptor proteins that cannot transport the male hormones correctly. Additionally, these defective androgen receptors are thought to accumulate in nerve cells and block normal processes. These defects lead to death of the nerves cells and loss of communication between nerve and muscle cells, leading to muscle dysfunction and the signs and symptoms of SBMA.
SBMA is considered an X-linked inherited disorder that primarily affects males, though in rare cases, it can affect females. The term X-linked refers to the fact that the AR gene is located on the X chromosome. Since boys are born with only one copy of the X chromosome, every boy who inherits an X chromosome with the defective AR gene will produce flawed androgen receptor proteins and be affected by the disease. Girls, on the other hand, are born with two copies of the X chromosome. Therefore, a girl who inherits one defective AR gene may still have normal copy of the AR gene on her other X chromosome and produce some normal androgen receptor protein. Girls with one copy of the mutated AR gene are known as carriers, and they can potentially pass on the defective AR gene to their children. SBMA carriers are usually asymptomatic, however, some SBMA carriers develop SBMA-like symptoms.
Diagnosis of SBMA
SBMA can be difficult to diagnose; the symptoms can be variable and the disease is sometimes mistaken for a more common condition, amyotrophic lateral sclerosis (ALS). An SBMA diagnosis is typically based on a combination of clinical symptoms and genetic testing. A specialized genetic test performed in a diagnostic laboratory is required to detect the trinucleotide repeat expansion in the AR gene and this test may be a prerequisite for enrollment in clinical trials. Genetic counseling and testing are important for individuals with a family history of SBMA or for those who are at risk of passing the condition on to their children.
Current management of SBMA
There is currently no known cure or disease-modifying therapy for SBMA. However, several therapies and strategies are available that can help manage the symptoms and improve the overall health of people with SBMA. These include:
- Physical and rehabilitation therapy to improve muscle strength and functionality
- Use of walkers, wheelchairs, and other adaptive equipment to help with mobility
- Occupational therapy to help develop skills and strategies to carry out daily activities with greater independence
- Speech/swallow evaluations and therapy to address difficulty speaking (dysarthria) and difficulty swallowing (dysphagia)
- Use of augmentative communication devices to address difficulty speaking
- Breast reduction surgery to address gynecomastia
Given the variability of disease progression and symptoms experienced by different people with SBMA, treatment plans are typically individualized to meet the needs of the affected person and may include recommendations from a variety of specialists.
Evolving research and treatment landscape
While the standard of care is still symptom management, research advances and the promise of better therapeutics on the horizon offer hope for people living with SBMA. Understanding of the genetic elements that cause SBMA have led to improved diagnosis and are guiding the development of new treatment strategies.
Both high-dose testosterone (introducing a lot of the male hormone into the body) and anti-androgen therapy (blocking male hormones in the body) have been tested as therapies for SBMA, but neither approach has been proven effective. Additional interventions are being explored in preclinical animal models. One promising drug candidate that has moved to the clinical trial stage is:
AJ201 (AnnJi Pharmaceutical Co., Ltd./Avenue Therapeutics) – AJ201 is a small molecule drug thought to have multiple beneficial effects in nerve cells, including the ability to block oxidative damage (toxicity due to harmful free radicals) and to promote proper protein folding, including folding of the androgen receptor. The safety, tolerability, and dynamics of this drug in people with SBMA are being studied in a phase 1/2 clinical trial.
Investigational therapies for SBMA are still in the early stages of development and may not be available for widespread use for some time. They represent promising areas of research, however, that could lead to new and effective treatments for SBMA.
Clinical trial readiness
In order to prepare for drug development in the SBMA field, some researchers are focusing on natural history studies to better understand the rate of disease progression and validate clinical outcome measures and biomarkers for use in future clinical trials. One such study is being conducted by the National Institute of Neurological Disorders and Stroke (NINDS) to collect information about SBMA disease progression over time. In this observational study, researchers will monitor people with SBMA every six months over a two-year period for changes in muscle strength and function, lung/breathing function, biomarker levels in blood and urine, and structural changes in the brain, as assessed by MRI, among other measures. This study is currently enrolling participants.
To learn more about clinical trial and natural history study opportunities in SBMA, visit clinicaltrials.gov and search for “spinal bulbar muscular atrophy” in the condition or disease field.
MDA’s work to further cutting-edge SMBA research
Over the last 30 years, MDA has invested more than $5 million in SBMA research. Recently funded projects include:
SBMA motor neuron degeneration: From cellular and molecular basis to therapy (2017-2020)
Dr. Albert La Spada, Duke University School of Medicine
Androgen Receptor isoforms: from SBMA pathogenesis to therapeutic targets (2018-2022)
Dr. Carlo Rinaldi, University of Oxford
These and other studies will help researchers identify new targets for therapeutic intervention and new biomarkers for use as reliable readouts for future clinical trials, thereby improving prospects for better disease management for people living with SBMA.
MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about spinal-bulbar muscular atrophy (SBMA), open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
Next Steps and Useful Resources
- For more information about the signs and symptoms of SBMA, a detailed clinical overview of SBMA can be found here.
- To learn more about clinical trial and natural history study opportunities in SBMA, visit clinicaltrials.gov and search for “spinal bulbar muscular atrophy” in the condition or disease field.
- MDA’s Resource Center provides support, guidance, and resources for patients and families, including information about spinal-bulbar muscular atrophy (SBMA), open clinical trials, and other services. Contact the MDA Resource Center at 1-833-ASK-MDA1 or ResourceCenter@mdausa.org.
- Stay up-to-date on Quest content! Subscribe to Quest Magazine and Newsletter.
TAGS: Clinical Trials, Fundraising, Grants, Healthcare, Innovation, Research, Research Advances, Simply Stated
TYPE: Blog Post
Disclaimer: No content on this site should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.




